Before Ann McKee talked about her research into concussions and brain disease in football players and other athletes, she wanted to correct any misconceptions about her motivations. “It’s not because I hate football,” McKee, whose work has alerted the public to the long-term dangers of repetitive hits in football and other sports, told an audience in Washington on February 25. “Football is in my blood,” she said.
“I was born and raised outside Green Bay, Wis., in the Vince Lombardi era. My brothers played football. My dad played. I was one and a half when they tried to get me to play,” said the School of Medicine professor of neurology and pathology. “I understand that it’s more than a sport—it’s a culture.”
McKee was speaking during a panel discussion on concussions, sports, and brain injuries in athletes and military members hosted by President Robert A. Brown at the Reserve Officers Association on Capitol Hill before an audience of more than 100 alumni, medical researchers, and congressional staff. Joining McKee on the panel were former New England Patriots and Los Angeles Raiders star Mike Haynes, and Jonathan Woodson, assistant secretary of defense for health affairs at the US Department of Defense (DOD). Moderating the discussion was Bob Tedeschi, a senior writer for STAT, an online health and life-sciences publication backed by the Boston Globe Media Partners, which has been publishing a continuing series on concussions.
“I care about the players,” said McKee, director of Boston University’s Chronic Traumatic Encephalopathy (CTE) Center. She showed the audience slides of the tiny tangles of a protein called tau that have been discovered, clustered around blood vessels, in the dissected brains of deceased football players with CTE, a neurodegenerative brain disease found in athletes with a history of repetitive brain trauma. “We want to do things that will protect their health,” she said.
“The culture of professional football today is completely different than when I started, because of people like Ann McKee and other doctors who are educating the public about CTE and concussions,” said Haynes, who was the Patriots’ first round draft pick in 1976. “The game is getting safer, it’s evolving. It’s not there yet.”

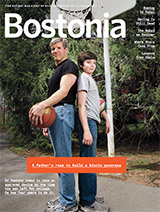
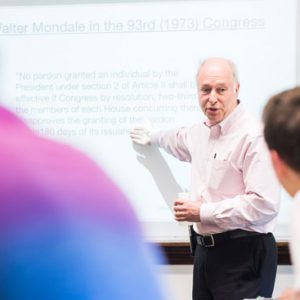
Tedeschi (right) with Haynes, who told the panel audience that college and pro football are now safer than youth football.
Haynes, wearing his gold Pro Football Hall of Fame jacket, told the audience that he has two sons, ages 12 and 16, who play youth football and high school football in California, where the family lives. Haynes coaches youth football.
“My fear is youth football,” he said. “College football and pro football are safer than youth football. In college and pro football there are people who monitor the games, monitor the hits. In youth football, we don’t have that. A player could knock a player out intentionally each week and no one would notice. He might get a 15-yard penalty, but he’ll stay in the game. My concern for youth football is what got me into coaching. I was not going to let my boys play for a crazy coach who was throwing kids out there because he didn’t know anything about concussions.”
McKee echoed Haynes’ worry. “Youth football is the most concerning,” she said. “It’s sort of the Wild West in youth football.”
However, the answer is not to shut down the game, she said. “We don’t want to stop our kids from playing sports. Team sports, exercise, is so important. We want to encourage sports, but in a smart way, so all our children and athletes can develop to their full potential.”
Both McKee and Woodson, who is a former MED associate dean of students, diversity, and multicultural affairs and professor of surgery, stressed the need for more collaborative and interdisciplinary research into brain injuries in athletes as well as in military members. “Concussion science is still largely unknown,” McKee said. “Right now concussions are judged by symptoms. We need a way to diagnose a concussion with a blood test or something easy we can do on the sidelines so we can follow a player and have an actual measure of brain injury.”
McKee, along with researchers at two other institutions, received a $6 million grant from the National Institutes of Health (NIH) in 2014 to set up a data bank to share their research on brains. McKee talked about her work on that grant, as well as the $16 million NIH grant awarded in December 2015 to BU’s CTE Center—with Robert Stern, a MED professor of neurology, neurosurgery, and anatomy and neurobiology, as the lead investigator—and a number of other institutions, to study CTE in living people. Currently, CTE can be diagnosed only by examining people’s brains after they have died.
“The biggest aim of the CTE Center is to be able to diagnose CTE during life,” said McKee, who listed some of the questions researchers are pursuing: “What factors make some people more resilient, or more susceptible, to concussions? Are there genetics that are important in this disease? We think there are. Do alcohol, drugs, opioids, steroids play a role? They probably do. We need to find out.”

Brown (left), with Woodson at Thursday’s panel discussion on brain injuries.
The panel discussion was organized by Jennifer Grodsky, the University’s vice president for federal relations, and her Washington office, as part of their work in connecting policy makers with BU researchers.
At the DoD, the Defense Centers of Excellence for Psychological Health & Traumatic Brain Injury is one of the areas under Woodson’s authority. “We’ve been at war for 15 years now,” he told the audience, and the signature injury is traumatic brain injury (TBI) caused by an IED (improvised explosive device). “Many of our men and women have been in blast zones. This is an issue of great significance for us. We need investigation and research into the long-term implications.”
The DOD is working with major academic research centers in an effort to develop effective treatments, improve diagnosis, and find ways to prevent TBI, Woodson said. It is essential that researchers collaborate and share data, he said, adding that President Obama has made the breaking down of research walls a priority of his administration.
Brain injury is caused not just during combat, but in training. “We jump out of helicopters and planes. The number of concussions in airborne units is significant,” Woodson said. The DoD is also working on addressing the stigma of reporting concussions. When it comes to how military members respond to concussions, he said, the culture is not all that different from the NFL: “They say, ‘Put me back in the fight, put me back in the game.’”
Sara Rimer can be reached at srimer@bu.edu.




































Related Stories
Could Pee-Wee Football Lead to Brain Injury?
MED study: more brain damage in NFL players who started playing early
BU-Led Study: CTE May Occur without Concussions
Progressive brain disease could be caused by repetitive head injuries
Football: Child’s Play, Adult Peril?
MED study: NFL vets starting football under age 12 at increased cognitive impairment risk
Post Your Comment