It was the bike ride seen ’round the world.
When Maine nurse Kaci Hickox hopped on a bike on October 30, openly defying a quarantine order to stay home after she returned to this country from treating Ebola patients in Sierra Leone, she intensified a legal and ethical debate likely to have far-reaching consequences in the United States. This according to a panel of BU and Massachusetts health experts convened on October 30 on the Medical Campus to discuss the Ebola outbreak.
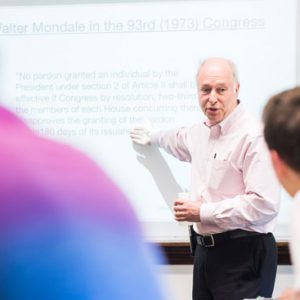
“There are actually two epidemics going on,” said panel member George Annas, a William Fairfield Warren Distinguished Professor and a professor at the Schools of Medicine, Law, and Public Health, where he is chair of health law, bioethics, and human rights. “There’s an Ebola epidemic in West Africa. And there’s an epidemic of ignorance in the United States.”
The US epidemic Annas was referring to was both the overblown alarm about Ebola and the resulting government actions, including the forced quarantine of Hickox, who was isolated in a tent at a New Jersey hospital for four days after she landed at Newark Liberty International Airport October 24. She tested negative for Ebola, but was ordered to self-quarantine when she was allowed to go home to Maine. On October 31, a Maine judge rejected state efforts to confine her in her home, but required her to submit to daily monitoring for the virus until November 10, when the incubation period for contracting the disease will be over.
Annas and four other medical and legal experts—two from the Massachusetts Department of Public Health (DPH) and two from BU—told the overflow crowd that the handling of Ebola, both in Africa and in the United States, has raised a host of ethical questions. The way the United States treats health workers returning from the three countries hardest hit by Ebola—Liberia, Sierra Leone, and Guinea—could have a profound effect on the willingness of others to help, and on the course of the disease, they said.
“The entire health care system is decimated” in these countries, said Nahid Bhadelia, who recently returned to the United States after treating Ebola patients in Sierra Leone. The MED assistant professor of infectious diseases, director of infection control at BU’s National Emerging Infectious Diseases Laboratories, and Boston Medical Center associate hospital epidemiologist said a lack of resources has contributed to the “exponential growth” of Ebola cases, and she stressed the need for more physicians and health care workers to assist.
“We just don’t have enough hands to help out,” said Bhadelia. “It’s the amount of work to be done and how few people there are” that’s fueling the death rate. There have been close to 14,000 reported Ebola cases and 4,922 deaths to date.
Bhadelia is now preparing to head to Liberia to treat patients there. She noted that the survival rate from Ebola is over 50 percent if it is caught in time. “This is a call to action for us,” she said. “Imagine what we can do with enough hands…which is why the discussion of health care workers here” is so important.
Annas and colleague Wendy Mariner, the Edward R. Utley Professor of Health Law, Bioethics, and Human Rights at SPH, a LAW professor of law, and a MED professor of sociomedical sciences, said a lack of clarity over which agency is in charge of Ebola has contributed to conflicting messages. The World Health Organization has come under fire for not sounding the alarm about Ebola soon enough and for not coordinating a response.
The US Centers for Disease Control and Prevention (CDC) recently issued guidelines that call for restrictions and monitoring of health workers who are at elevated risk of infection, but stopped short of the strict quarantines that some states have imposed. Meanwhile, the Department of Defense has announced that troops returning to this country after deployment to West Africa will be isolated for 21 days—the incubation period for Ebola—even if they are symptom-free.
“I don’t know who’s in charge,” Annas said with a shrug. “There’s a vacuum of leadership.”
Several states are imposing quarantines on health workers who have had contact with Ebola patients. Mariner said that while states have broad powers, there are constitutional limits on when citizens can be confined: they must have a serious contagious disease and there should be a probability that they will transmit the infection to others.
“That second point is being lost,” she said.
Mariner said of New Jersey and the other states imposing strict quarantines, “When you hear somebody say it’s out of ‘an abundance of caution,’ you know they have no facts behind them.”
She said Massachusetts, which is not imposing mandatory quarantines, is “doing a good job–but they’re a rare bird.” The state has had no reported Ebola cases.
“We need courageous public health and legal officials…who won’t be bullied” or swayed by fear, she said.
Two Massachusetts DPH officials addressed criticism that the agency had not done enough to help to prepare for Ebola, saying the department is working closely with hospitals and emergency responders, while also trying to allay fears of contagion. The agency is in discussions with hospitals about whether to create regional Ebola-specialty facilities.
Alfred DeMaria, state epidemiologist and medical director of the DPH Bureau of Infectious Disease, said that even if some hospitals are deemed regional centers, the entire health care system needs to be prepared to deal with cases.
“Patients aren’t going to go to an ‘Ebola hospital’” when they have symptoms, DeMaria said, but would likely go to the nearest hospital or health care provider, so “we still need to build a system” of community providers trained and equipped to treat Ebola.
All state hospitals have invested in training and equipment to prepare for the possibility of an Ebola patient, according to the state officials. Boston Medical Center is building a three-bed biocontainment unit that is expected to be ready in mid-2015.
DeMaria said that the DPH is following CDC recommendations that any identified, higher-risk residents restrict their interactions and undergo active monitoring for symptoms and fever at least once daily.
“We’re going to be very diligent in applying the least restrictive measures…while ensuring the public’s health,” he said. The country should be embracing health care workers returning from West Africa “with gratitude, not shutting them in and locking them up.”
The department has been trying to allay fears that the virus, transmitted through bodily fluids, is airborne or easily spread, DeMaria said. He noted that the one person who has died of Ebola in the United States, in Texas, had possible contacts with more than 100 people, but that 2 nurses who treated him at the end stage of his illness were the only ones who had contracted the virus.
“Distance is your best protection,” he said.
Mary Clark, director of the DPH Office of Preparedness and Emergency Management, said the agency began working with health care and emergency providers in August to prepare for Ebola cases. The DPH has set up a special email account for residents who have questions about Ebola: AskEbola@state.ma.us.
An audience member at the forum asked panelists why Ebola had attracted so much more public attention than illnesses such as malaria and pneumonia, which claim many more lives in Africa.
Initially, Mariner answered that those other illnesses have been around so long that people have grown tired of hearing about them. Then she added that it was also because Ebola has “jumped here.”
Annas agreed. He said he hoped the Ebola outbreak ultimately might lead to better health care for people with other diseases, if health systems in those West African countries are strengthened.


































Related Stories
Going Public with Ebola
NEIDL director says scientists need to engage with the public about the disease
Battling Ebola: The Ethical Issues
Experimental drug use treatment at heart of the debate, says BU’s Annas
How Ebola Kills
MED’s John Connor is devising diagnostics to spot Ebola and antivirals to treat the disease
Post Your Comment