When Jerrold Ellner started working in infectious disease, schistosomiasis was a greater concern to international health professionals than tuberculosis. Fast forward a few decades and TB is now among the greatest public health threats worldwide.
There are nine million new cases and three million deaths annually from the disease, says Ellner, a School of Medicine professor of medicine and chief of Boston Medical Center’s infectious diseases section. Most troubling is that 500,000 of these cases are multidrug-resistant, meaning they don’t respond to the most effective antibiotics and are more complicated and expensive to treat. An overwhelming majority of these cases and almost all deaths occur in resource-limited nations.
One third of the world’s population has had a positive skin test for tuberculosis, but only 5 percent of those who test positive move from a latent to an active infection. The mystery for scientists like Ellner is: which 5 percent? Right now, he and his colleagues have no way of identifying these individuals, who are essentially the needles in a haystack of two to three billion people.
The good news is that once people develop active TB, the vast majority of them can be cured with a six-month regimen of antibiotics. Those TB infections that are multidrug-resistant require a more toxic cocktail of antibiotics over a longer period of time, up to 24 months for particularly stubborn cases. People fighting drug-resistant TB in developing nations usually must quit working, travel long distances to medical facilities, and adhere strictly to a costly drug regimen that often has debilitating side effects, but no guarantee of a cure. It’s enough to make patients throw in the towel before treatment is complete, and make doctors wish there were a concrete way to determine when a patient is cured.
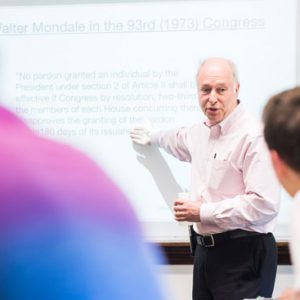
Resolving these two issues—finding a way to identify which people with a latent TB infection will develop an active case, and determining an endpoint for successful TB treatment—are the goals of a seven-year, $21 million grant that Ellner and his international team of scientists received from the National Institutes of Health last summer. Their research is divided into four projects; two studying latent and persistent TB in humans in Brazil, China, and South Africa, and two studying latent and persistent TB in rabbits, which, Ellner says, “reflects human disease and allows us to look at drug treatment and penetration into tissue in lesions.” The lab work will also help scientists answer key questions about the bacteria’s genetics and how or where the disease strikes.
“What I consider the current Holy Grail of TB research is a biomarker that you could use to take someone that you know is infected with TB and predict that this person is at risk of developing active TB,” Ellner says. “If we could say this person is at risk or this person is cured, we could talk about treatment, or preventive therapy.”
If Ellner’s team is successful, TB could be the world’s next polio. “We could eliminate TB by 2050,” he says. “If you can eradicate the latent reservoir, it means you prevent further transmission. When people reactivate their TB, they infect another 20 people, and then the problem exists for another generation. But if you treat the people and prevent them from developing infectious TB, then you can really stop it.”
Brazil, South Africa, and China were chosen as research sites because of TB’s large presence in their populations, Ellner says, and because they are middle-income countries with strong research infrastructures. South Africa and China have a greater percentage of multidrug-resistant cases, while Brazil has more cases that respond to first-line antibiotics. “There’s so much TB in these countries,” he says, “and you’d rather work in an area where it’s a major public health problem, because the things that you find will be relevant in those populations.”
Patients will be followed over the course of their treatment at each site. Researchers will collect blood samples and conduct PET/CT scans, which detect inflammation in soft tissues like the lung and lymph nodes. “The more activity on PET scans, the more likelihood of a patient developing active TB down the line,” says grant coinvestigator Karen Jacobson, a MED assistant professor of medicine.
Ellner’s Holy Grail could help resolve the mystery of the 5 percent whose latent infections will become active. “If we could try to identify the many infected and target preventive therapies for those few, then we’d really be in business,” says Edward Jones-Lopez, a MED assistant professor of medicine, another grant coinvestigator.
For patients already undergoing treatment for active TB, “PET scans could be used as interim indicators of relapse,” Jacobson says. “We could find biomarkers in the blood to correlate with these PET scan results. Blood biomarkers could then be used to better stratify who looks really cured versus who’s more at risk of relapse.” Doctors could then adjust treatment regimens to fit patients’ progress.
“We hope that we can eliminate the disease in the United States and then abroad,” says Robert Horsburgh, a School of Public Health professor of epidemiology, biostatistics, and medicine and a member of Ellner’s team. “But without better tools, we’re never going to make any progress eliminating it in the rest of world. We did it with smallpox and polio, and we’d like to do it with TB.”


































Related Stories
Khalil Wins NIH ‘New Innovator Award’
Project will focus on combating antibiotic-resistant bacteria
NEIDL Researchers Present Case for Next-Level Research
Tell Boston Biosafety Committee that BSL-4 work will speed development of new vaccines and cures
How Bad Drugs Turn Treatable Diseases Deadly
Low-quality and counterfeit antibiotics drive drug-resistant infections
Post Your Comment