Idiopathic condylar resorption. A meaningless medical mouthful to most people, ICR is all too real for Holly Anderson. Left untreated, the rare medical condition could someday take her life.
Which is why, three weeks before Christmas 2015, the 21-year-old Bridgewater State student and veterinary technician from Taunton, Mass., lies in a blue hospital gown on a mobile bed off Boston Medical Center’s pre-op area, her parents, Rick and Claire, quietly chatting with her. A dozen years of living with the progressive condition and its consequences—braces, countless visits to specialists, painful surgery—could end, starting today.
ICR affects less than one percent of the population, mostly teenage girls, says Anderson’s surgeon, Pushkar Mehra (SDM’95,’99). It’s a gradual dissolving of the jaw’s hinges that causes the lower jaw and chin to droop farther and farther. “If you saw the X-rays of her jaw and everything, it’s actually cutting off her windpipe,” her father says. Anderson used to wake up nights gasping for air, so she now props herself on lots of pillows in bed, practically sitting, so she can breathe while sleeping. Her falling jaw causes a small but uncloseable gap between the upper and lower teeth, making it difficult to eat. Her profile reveals a noticeably sagging chin.

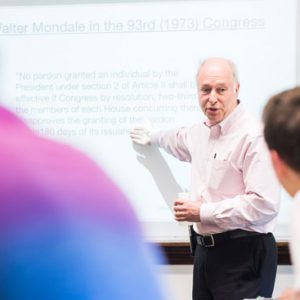
Pushkar Mehra, a Goldman School of Dental Medicine professor and a BMC surgeon, replaced the hinges of Holly Anderson’s jaw to fix a potentially life-threatening deterioration. Photo by Dana Quigley
If her condition is rare, so too are Mehra’s credentials. A Henry M. Goldman School of Dental Medicine professor and chair of oral and maxillofacial surgery, he says conventional treatment would require Anderson to undergo up to three surgeries to reconstruct her jaws with artificial hinges. Mehra is among a handful of surgeons who can do it in a one-step, 10-hour operation, replacing her jaw joints with artificial ones and repositioning the upper and lower jaws to close her bite. (One teenage girl came from France to be operated on by Mehra.)
Now, on surgery day, he walks in at 10:30 a.m., a white lab coat covering his blue scrubs. He asks if Mom or Dad have any questions. “Just take good care of her,” her father says. “We will,” Mehra promises. Because of post-op pain and discomfort, he says, “she’s not going to like me for six, seven days. Then we’ll be friends again.”
It’s time. Rick kisses his “little girl,” the younger of his two children, who’ll be staying two nights in the hospital postsurgery. “I’ll be here,” her mother promises her.
At eight minutes past noon, Anderson is wheeled into an operating room.
Whiz-bang technology and exquisite surgical skill
The trajectory that led the lives of doctor and patient to cross began for Anderson a dozen years ago in fifth grade, when she was outfitted with braces for nine months. “As soon as they came off, my mouth started having the open bite,” she says. As it worsened, “I felt like I looked stupid. I think the worst part of all of this was putting braces back on” in 2014. As a college student, she had to take public speaking. Giving an address in braces, she says, “I look like I’m 12.” At work, where she’s a head veterinary technician, many clients “think I’m, like, a little kid, so they don’t believe me when I’m talking to them about something.” A round robin of orthodontists finally steered her to Mehra. “He knew what it was, but everybody else had no idea,” Anderson says.

To design Anderson’s new jaw hinges, Mehra worked with a model of her real jaws. Photo by Dana Quigley
Mehra had performed the first of these one-stop surgeries in 2001. He learned the technique, even though ICR is rare, because it helps him to do more common surgeries for other deformities or injuries. “Till about two, three years ago, there were probably less than 15 people in the country doing this surgery,” he says. He has mastered making small, unobtrusive, centimeter-or-so incisions at the ear and by the neck. With just one operation, he says, “we can save the patient three general anesthetics, three hospitalizations.”
It’s a lot of work, though. To make sure the titanium alloy hinges that would replace Anderson’s God-given ones were sized properly for her jaws, Mehra first sent a CT scan of Anderson to a California medical company—it makes “the Rolls-Royce of joints,” he says—which constructed a two-piece acrylic model of her upper and lower jaw for Mehra.
Using computerized mapping of Anderson’s actual jaw as a guide, Mehra manipulated the model and took measurements for the artificial hinges to correctly size them so that the model closed properly, with no teeth gap. This ensured that they’d work once he implanted them in Anderson’s skull. He then sent the model and his measurements back to his California collaborators to make the hinges, each a two-centimeter-long plastic socket with a titanium shell that attaches to the cheekbone by the temple.

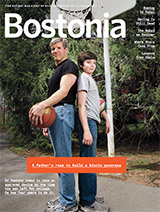
Surgery day: Anderson, her mother, Claire, and father, Rick, moments before she underwent the 10-hour surgery. Photo by Dana Quigley
Whiz-bang technology and exquisite surgical skill weren’t enough, however. Mehra had to tap old-fashioned bedside manner to coax Anderson into the OR. She had wearied of years of orthodontist visits and feared a repeat of her unpleasant recuperation following a 2013 surgery, when Mehra inserted a palate expander in her upper jaw so that it would align with her lower jaw—desirable if her bite were to be closed later.
“Nothing worked for pain afterward,” she says. “You vomit blood for, like, weeks. My nose bled for three months.” Pumped full of medication, she lost her appetite. To install the palate expander, the doctors had to cut her jawbone and the roof of her mouth; twice a day, she had to take a wrench and crank the device two turns, slightly spreading her two front teeth apart to allow new bone to grow.
Then last year, frustrated by a feuding relationship with her orthodontist and years of wearing braces, Anderson says, she “almost quit.” She made an appointment to have the braces removed, “but then he tattletaled and told Dr. Mehra, who called me at work and told me, ‘You’re not quitting. Just suck it up with your orthodontist.’ He gave me his whole little speech about how I’m a running car, and I’ll break down” without the surgery. “Dr. Mehra helps me get through every obstacle.”
“She looks beautiful”
Mid-April, four months after the operation: Anderson has returned to Mehra’s office for a checkup. He high-fives her on entering the room, where he measures the proportions of her face. A lot has changed.

Four months after surgery, the looks on the faces of both doctor and patient testify to the operation’s success. Photo by Jackie Ricciardi
She’s still slightly swollen from the surgery. “At school, no one knew who I was,” she says. When she first looked at herself in the mirror, “I was so mad. I was like, I look like a man.” Her spirits have rebounded, for good reason: her bite is now closed. She’s shed the braces. Seen from the side, her chin is sharper and more defined. Plus, pain medications worked much better following this surgery than they did after her palate-expanding operation.
After existing on a liquid diet for almost two months post-op, Anderson was happy to be reintroduced to real food. Pillows stacked high for sleeping? Gone.
Mehra asks if she’s having any aftereffects, like headaches. Negative, she tells him. The doctor says he’ll see her in a year for the next checkup. “Every year, we’re going to have an anniversary,” he quips.
For now, his patient says, “Everything’s perfect.”
“She looks beautiful,” her father says.
Bill Politis can be reached at
bpolitis@bu.edu.







































Related Stories
School of Dental Medicine Celebrates 50th Anniversary
Home to scholars, community activists, and miracle workers
Changing Face of BU Athletics Creates Buzz
Marked by a change in sports league and a state-of-the-art field,
Boston Globe takes note of new era
Rare Double Arm Transplant for Former COM Lecturer
Will Lautzenheiser is reminded how great a hug can feel
Post Your Comment