As far as age-related fractures go, broken hips are the injury that people fear most—the one that could end your life as you know it, or end your life, period. But while broken hips garner the most attention, spine fractures are far more common, affecting approximately 25 percent of all postmenopausal women in the United States, according to the journal American Family Physician. The prevalence of these fractures rises as we get older, affecting 40 percent of women who reach age 80 and nearly 20 percent of men over the age of 50. And the consequences can be serious: back pain, height loss, hunched posture, and immobility.
Spine fractures are insidious because many go undiagnosed, brushed aside as the back pain that comes with getting older. But they indicate risk for even more spine fractures, and hip fractures as well. If a doctor misses someone at high risk, the patient may have more—and worse—broken bones down the road.
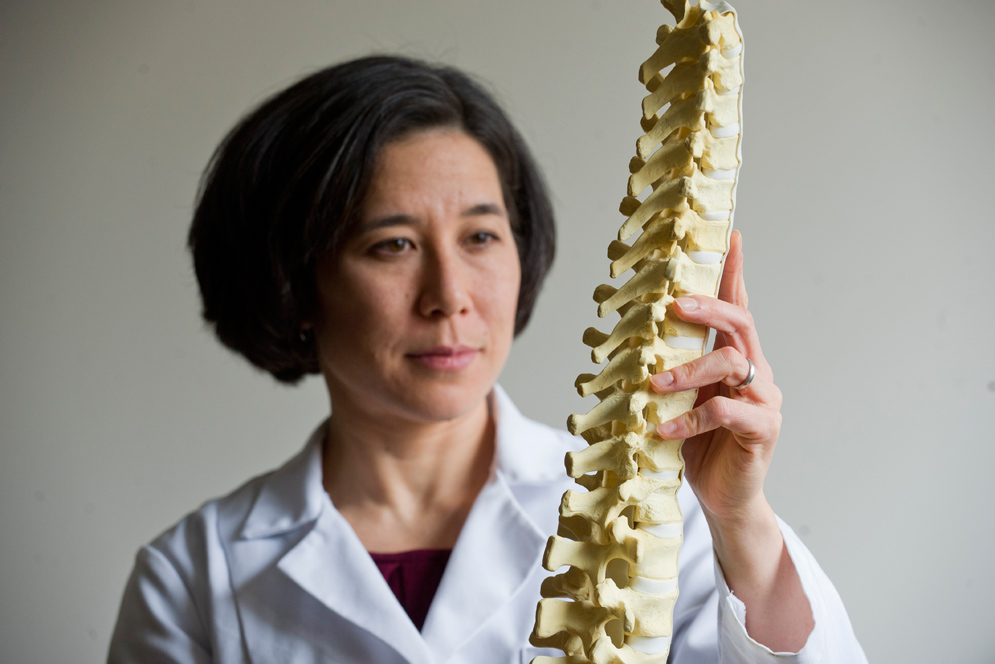
Despite the big numbers and enormous consequences, age-related spine fractures remain difficult to predict, so people who might benefit from preventive treatment often don’t get it (and some people who do get treatment may not need it most). Elise Morgan, a College of Engineering professor of mechanical engineering, wants to change that, by finding a better way to predict age-related spinal fractures. “We’re trying to develop methods for identifying who is really at risk for fracture,” she says, “methods that are much better than what’s currently used.” She’s doing it in an unusual way, by using the tools of mechanical engineering, techniques more commonly used to measure stress and strain on bridges and buildings.
“Elise’s engineering background gives her a fundamental understanding of mechanics, which informs every part of her work,” says Paul Barbone, an ENG professor of applied mechanics and theoretical acoustics who collaborates with Morgan. “She can look at the problem from both sides: how do the bones hold up as a structure, and how does bone growth and development play a role? It gives her a unique perspective.”
Doctors currently assess a patient’s risk of spine fracture with a bone density scan, basically an X-ray that measures how much bone you have and how dense it is. The scan generates a “T-score,” which classifies a person’s bone density as compared to the rest of the population. Using the T-score, a doctor categorizes you as either normal, osteoporotic, or “osteopenic”—a term meaning almost-but-not-quite osteoporotic. The problem, says Morgan, is this: about half the people who fracture their spine are classified as normal based on their T-score. “Clearly the scan is missing something,” she says.
Morgan and her team, with funding from the National Institutes of Health (NIH), want to develop a screening technique that’s better able to predict who will actually fracture. That’s difficult, though, because it’s not always clear how spines fracture. That’s where Morgan’s engineering background comes in.
“As a mechanical engineer I’m thinking, well, we’ve got this exquisite structure that is the spine, and even a single vertebra itself is a fairly complicated structure,” she says. “The first thing we need to do is really understand how these fractures occur. Otherwise, it’s hard to predict whether they will occur. And so that’s really a mechanical engineering problem: How is a structure failing?”
To answer this question, Morgan and her colleagues took human vertebrae, from people who donated their bodies to science, and squeezed them until they broke. This type of testing is unusual: typically, when engineers want to examine the mechanical properties of a material, they take small samples and craft them into a standardized size and shape for testing. This makes sense for, say, titanium alloys, but not for bone. “Bones don’t come in standard shapes and sizes, and the properties of the tissue vary throughout the bone,” says Barbone. Testing whole vertebrae, he adds, “is like testing hundreds of samples, all at once, in their native configuration, interacting with their neighbors as they would normally.”
In the video above, researchers in Morgan’s lab crush vertebrae to learn exactly how they fail. “The first thing we need to do is really understand how these fractures occur,” says Morgan. “Otherwise it’s hard to predict whether they will occur.
Morgan’s team squashes the vertebrae using a pair of machines that not only measure force and deformation but also grab images of the vertebrae with a micro-CT scan. “We do that imaging while we’re doing the mechanical testing, so we get time-lapse series of images of how the vertebrae are failing,” says Morgan.
Much of the original testing fell to Amira Hussein, a postdoctoral fellow on BU’s Medical Campus who worked on the project as a PhD candidate in Morgan’s lab. “The human skeleton is a mechanical system but it grows and adapts in response to stress, so everyone’s vertebrae are different,” she says. “That’s really cool.”
Morgan’s team used computational tools developed in Barbone’s lab to interpret and analyze the image data. Hussein says this step was critical for finding exactly when and where a vertebra “failed,” or lost its ability to support a load. “Once we could see where the failure took place,” Barbone says, “we looked to see what was special about the structure of that part of the bone. Was there anything different that could help us predict fracture?”
The tests revealed some surprises, says Morgan. They found that almost all vertebrae failed when depressions and cracks appeared in the center of the top endplate—the flat circle of bone tissue that caps each vertebra—rather than in the very low density bone inside. It didn’t matter if the researchers tested vertebrae from the lower or middle portion of the spine, and it didn’t matter if the machine squeezed the samples vertically or flexed them in an arch, the way the spine bends when someone reaches down to pick up a bag of groceries—the vertebrae all failed on the top endplate. But why there?
Further investigation showed that the endplate tended to fail first where it was the most porous, with the weakest internal microstructure. While one might expect weak, porous bone to fail first, nobody had experimentally identified this link between endplate microstructure and failure of the entire vertebra. This finding may prove useful for diagnosis, says Morgan: doctors viewing X-rays and CT scans of patients’ spines often report depressions of the top endplate, she says, a finding that may likely indicate a spine fracture. The research, conducted mainly by Hussein and her fellow graduate student Timothy Jackman, was published in the Journal of Orthopaedic Research in July 2014, with follow-up studies set to appear this year.
Morgan’s team used this data to build computer models that simulate spine fracture, models that led them one step closer to a predictive test. “With the 3D imaging, we were able to see the whole volume of the vertebra and where it fails, and then to compare this to the model to determine whether the model is working correctly,” says Hussein. “That was a major contribution.”
Morgan is now using CT scans from Framingham Heart Study participants—a large and well-established study group—to further test and refine her diagnostic model. She hopes that in a few years, this data may supply enough information to create a reliable test.
“Right now it’s really hard to identify who is being over-treated for osteoporosis, and who’s not being treated at all but should be,” says Morgan. “We want to change that.”



































Related Stories
The Bone Mender
A mechanical engineer works to help heal fractures, correct deformities
Thin Rod Study Wins NSF Grant
Douglas Holmes looks at potential for smart needles, robotic arms
Two from BU Cited for Encouraging Women in STEM
Lauded by magazine for their inspiration
Post Your Comment