Breast cancer is not color-blind. Although it strikes women (and less commonly, men) of every age and race, black women are more likely than white women to die of breast cancer.
Researchers have been aware of the disparity for decades, but it has resisted easy explanation. And today, the stakes are higher than ever. That’s because breast cancer rates in black women are rising, even as they are dropping for white women. White women were about 15 percent more likely to be diagnosed with breast cancer than black women 15 years ago, probably because they were more likely to be screened, typically had children later, and took more postmenopausal hormone supplements, which feed the types of breast cancer more common in white women. Now, as many women have chosen to cut out those postmenopausal hormones, the lines have converged, with women of both races equally likely to develop the disease. But on average, black women are diagnosed at a younger age (median age is 58 for black women, 62 for white women) and die at a younger age than white women (median age is 62 for black women, 69 for white women).
Researchers at BU’s Slone Epidemiology Center are building on a two-decade legacy of black women’s health research to understand the breast cancer survival disparity. With support from the National Cancer Institute, they are combining expertise in genetics, biology, and epidemiology and the social factors that influence health to search for answers that will illuminate how breast cancer takes hold and proliferates in the body—and how we might be able to prevent and treat it more effectively, not just in black women, but in everyone.
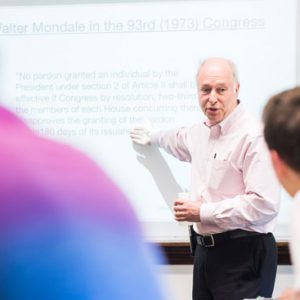
“Black women have a 42 percent higher rate of death from breast cancer than white women or most other groups in the United States, and we don’t know the reasons for that,” says Julie Palmer (SPH’85), a School of Public Health professor of epidemiology and Slone Center associate director. “What we do know is that it can’t be attributed to poor care or coming to diagnosis later. There’s clearly something going on that’s different.”
A letter in the mail
In 1995, a woman named Vi Brown got a letter in the mail. “Dear Friend,” it began, “We are delighted to inform you that the US National Institutes of Health has recently provided funds for the largest ever long-term study of the health of African-American women. There has been little previous research, and this study will provide much-needed information on causes of illness.” On the left was the seal of the Boston University School of Medicine, on the right, the shield of Howard University College of Medicine, and between them, in bold, double-underlined type, the name of the new project: The Black Women’s Health Study (BWHS).
Folded inside the letter was a 14-page survey dense with questions about the recipient’s medical history (Had she every been diagnosed with cancer? Heart disease?), her life story (Did she have any children? If so, had she breastfed them?), and lifestyle (Did she smoke? Drink? Eat vegetables?). The letter went out to more than 100,000 women, and Brown was among the 59,000 women who returned it.
Then in her mid-30s, she had actually read about the study in Essence magazine. “I never knew back then that they had not done a comprehensive health study on African-American women,” she says. “I thought, well, gee, why not?” Brown, who now works as a business and engineering consultant and owns her own company, reached out to the organizers, and the letter arrived shortly after.
When she volunteered, she had never had any serious health problems. But just two years later, she was diagnosed with early-stage breast cancer. She is now celebrating nearly 20 years of being cancer-free, and is encouraged by the move toward personalized medicine informed by a patient’s gender, race, and background. “The more we know, the more specific we can be in making sure the person is getting the right treatment,” Brown says.
Read the full story on BU Today



































Related Stories
Patient Navigators Improve Delivery of Care for Breast Cancer Patients
BMC program reduces cancer disparities by addressing barriers to timely care
Dioxins Point to Targets for Treating Breast Cancer
SPH’s David Sherr follows toxins’ trail to understand aggressive cancers
Zebrafish Cancer Genetics Illuminate Human Breast Cancers
MED’s Hui Feng focuses on MYC gene
Post Your Comment