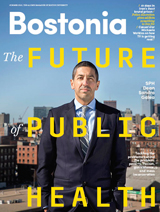
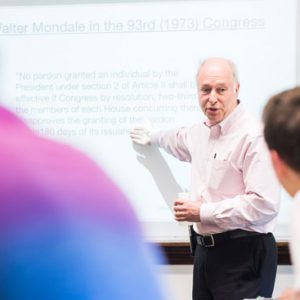
Muhammad Zaman learned at an early age that one did not shop for medicine at the convenient neighborhood pharmacy. In Pakistan, where he grew up, the safer thing to do was walk the extra mile to a pharmacy whose drugs were known to be high quality.
Four decades later as a College of Engineering professor of biomedical engineering, Zaman was reminded of the dangers of low-quality drugs in his native country when he learned that more than 200 people in the city of Lahore died after being treated with an adulterated version of a hypertension drug.
That event, in 2012, altered the course of Zaman’s research. Now, he focuses on the global problem of “substandard drugs,” poorly made medicines containing ingredients that are either ineffective or toxic. His most recent discovery has startling implications for our understanding of drug resistance: a low-quality version of rifampin, a broad spectrum antibiotic typically used as the first line of defense to treat tuberculosis, can greatly contribute to the development of drug-resistant infections.
The findings, published in Antimicrobial Agents and Chemotherapy, are particularly pressing because drug-resistant TB is an increasing problem worldwide. Of the 10 million new cases of tuberculosis in 2016, about 600,000 were rifampin resistant, requiring second-line treatments which come with increased toxicity.
“There had not been a definitive study showing that lack of [antibiotic] quality leads to resistance,” says Zaman, who is also a Howard Hughes Medical Institute Professor of Biomedical Engineering and International Health. “Now we are sure that it does, and it does with TB, a global problem that has become stubbornly hard to resolve.”
“We had always thought of this a scientific issue, but now it is also an ethical issue.”
Muhammad Zaman
Zaman says substandard drugs, as well as drugs that are deliberate counterfeits, are all too common in developing nations. A recent survey by the World Health Organization found that in low- and middle-income countries, one in 10 medicines is substandard or falsified. One contributing factor could be that government enforcement of safe manufacturing practices is feeble or nonexistent. In Pakistan, for example, a country of nearly 200 million people, only a handful of federal inspectors monitor the quality of drug manufacturing.
Across sub-Saharan Africa, things are no better. A recent World Health Organization (WHO) study written in part by Paul Newton, a School of Public Health adjunct professor, found that substandard antimalarials killed more than 120,000 children under the age of five in 2013. Another WHO study, conducted in 2008, found that 64 percent of antimalarial drugs tested in Nigeria were substandard. When the same study looked at antimalarials in Cameroon, Ethiopia, Ghana, Kenya, Nigeria, and Tanzania, it found that 28 percent of 267 samples were substandard.
Zaman says it’s impossible to know how many deaths globally are caused by substandard drugs because people don’t usually die immediately. They could die, as the Lahore victims did, from a toxic reaction, or they could die from the disease that the drug was supposed to cure.
Or, says Zaman, he and other scientists have long speculated that they could die for a third reason: adulterated medicines could encourage the development of drug resistance, rendering the disease incurable with standard treatments. Although that possibility had been considered for years, Zaman and Zohar Weinstein teamed up to finally put the hunch to the test.

Researchers at Boston University have found a link between low-quality antibiotics and increased drug resistance in the bacteria (pictured here) that causes tuberculosis. Image courtesy of NIAID
In the lab, Zaman and Weinstein, a postdoctoral researcher in biomolecular pharmacology who’s nearly finished with her medical degree as well, conducted several tests with rifampin to learn if a degraded form of the TB drug could build drug resistance in bacteria.
They first ran a series of in vitro tests pitting rifampin against E. coli, sometimes referred to as the workhorse bacteria of laboratories because its rapid doubling time makes it ideal for such studies. The researchers exposed the bacteria to gradually increasing doses of rifampin, which suppresses RNA transcription in bacteria, leading to cell death. They then ran the same tests with rifampin quinone, the most commonly found form of degraded rifampin. Within a week, they observed that the bacteria became significantly more resistant to the drug.
Next, the researchers repeated the experiment, swapping out E. coli for a strain of tuberculosis called M. smegmatis, selected because it has a conveniently short doubling time of two hours, while the more common strain of tuberculosis has a doubling time of about one day. After two weeks, the M. smegmatis also began to show signs of resistance.
“We found that over five days, E. coli exposed to [rifampin quinone] became up to 64 times more resistant to rifampin,” says Weinstein. “And over 22 days, M. smegmatis became up to 100 [times] more resistant to rifampin.”
“You could be a good patient and still acquire drug-resistant bacteria, because the drugs you were taking were leading you to resistance.”
Muhammad Zaman
Zaman and Weinstein had expected such responses, but they didn’t expect to find such a powerful resistance. In fact, once the bacteria gained resistance, no amount of standard rifampin would kill them.
The researchers also looked for another indicator of rifampin resistance: a genetic mutation in a gene called rpoB. What they discovered was alarming.
“We found that the majority of bacteria exposed to [rifampin quinone] also had mutations in this gene, even though they had never been exposed to the standard drug,” says Weinstein.
In other words, the degraded drug wasn’t just failing to cure the disease, it was cultivating cross-resistance to the high-quality, standard product. In that sense, says Zaman, bad drugs can become doubly dangerous.
“That [observation] was very revealing,” says Zaman. “It changed the equation, because we had always thought of this a scientific issue, but now it is also an ethical issue. We usually think of the spread of resistant TB in two ways. We say you got it because you were exposed to resistant TB, maybe you were living with someone with resistant TB. The second way is you got it because you were supposed to take drugs and you didn’t adhere to the program. But what this study reveals is that you could be a good patient and still acquire drug-resistant bacteria, because the drugs you were taking were leading you to [treatment] resistance.”
“While it is well established that subtherapeutic doses of medicines play a role in antimicrobial resistance, this is, as far as I know, the first demonstration of how substandard medicines directly drive the emergence of resistance genes in pathogens,” says Michael Levy, vice president of USP’s Quality Institute, which researches the influence of substandard drugs on health outcomes. USP is a nonprofit organization that sets drug quality standards that are legally recognized in the US and are also used in more than 140 other countries.
Zaman’s next steps will be threefold. First, he plans to test the quality of drugs that are available in the community hospitals of several low-income countries, looking specifically for the presence of rifampin quinone, the degraded form of rifampin. Second, he plans to work with researchers at the National Emerging Infectious Diseases Laboratories (NEIDL) on a mouse model to study the resistance mechanism in vivo. Third, he says he hopes to expand his work to investigate adulterated forms of other commonly used, high-impact antibiotics.
Meanwhile, patients around the world are still being prescribed substandard antibiotics every day.
“The patient may be doing everything he or she is supposed to do and still become resistant [to treatment],” Zaman says.
This work was supported by National Institute of General Medical Sciences and USP.




































Related Stories
BU Researchers Work against Deadly, Disfiguring Disease
Pharmaceutical giant GSK chooses team in its new competition
Counterfeit Drug Screener Wins National Award
Promises to save lives in developing countries
Setting the Stage for Smarter Drugs
CAS biologist pioneers techniques leading to better disease treatments
Post Your Comment