Every year, an estimated one out of every 1,000 patients receiving general anesthesia for surgery—up to 40,000 people—will wake up unexpectedly during the operation. The problem, called anesthesia awareness, is a harrowing and painful experience that can haunt a patient for years.
“Although anesthesia is used all of the time, almost no one understands how it actually works,” says Nancy Kopell, a William Fairfield Warren Distinguished Professor and a College of Arts & Sciences professor of mathematics, coauthor of a recent paper on the subject.
Until now, scientists have not been able to identify the specific electroencephalography (EEG) patterns that mark the points when a patient loses and regains consciousness. Kopell, working with a group led by researchers Emery N. Brown of MIT and Massachusetts General Hospital (MGH) and Patrick Purdon of MGH, has done just that. Kopell’s research has also led her to surprising insights into other neurological disorders, among them Parkinson’s disease and schizophrenia.
“We think that every neurological disease is, one way or another, associated with pathologies in these rhythms,” says Kopell, recipient of a MacArthur “genius” award in 1990 and codirector of the Center for Computational Neuroscience & Neural Technology. “We can’t prove it yet, but that’s a working hypothesis.”
In the study of EEG patterns, published online in the March 2013 edition of PNAS Plus, the researchers collected the EEG signals of volunteers as they were given steadily increasing and then decreasing doses of propofol, one of the most commonly used anesthetic drugs, over the course of two hours. During that time, the volunteers responded to questions and auditory clicks. As the drug dose increased, the subjects were less able to respond to stimuli, until finally there was “a functional loss of consciousness,” Kopell says.
Scientists had long assumed that there was something in the brain that switched off at this point, plunging a patient into unconsciousness. But the group’s work showed the opposite. They discovered that when a person loses consciousness, a new set of rhythms emerges.

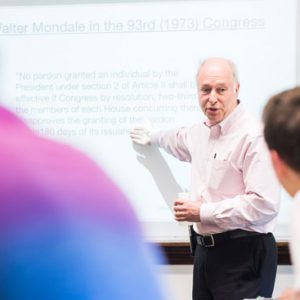
Nancy Kopell creates mathematical models to recognize when a patient loses and regains consciousness. Photo by Kalman Zabarsky
Kopell and ShiNung Ching, a BU postdoctoral associate, created computer models showing that the anesthetic leads to abnormal synchrony among brain regions, which impedes normal processing; they think the inability of regions to signal one another in normal ways is a critical reason for the loss of consciousness. The researchers also discovered specific sets of EEG signals for deep anesthesia.
Based on the new data, Purdon’s team at MGH is building a sensor that will collect an unambiguous real-time signal telling anesthesiologists when
a person is in a state of deep unconsciousness and warning them when a person is about to wake up.
Kopell’s role on the research team is different from that of a physician or a biologist. She is a mathematician-turned-neuroscientist who translates data into physiology. “I’m the bridge,” she says. “My role is neither to collect the data nor to analyze it, but to stare at it, make mathematical models, and suggest what might be going on physiologically.”
Her work on anesthesia awareness is part of a larger interest in cognitive rhythms, a growing field of study that examines how the brain’s electrical wave patterns contribute to sensory processing, motor planning, behavior, and cognition. Several years ago she founded the Cognitive Rhythms Collaborative, which gathers an interdisciplinary team of researchers from the Boston area to work on the subject from different angles.
Kopell first became interested in pattern formation in biology in the late 1960s, but the field was immature. Looking for a testable problem, she turned to chemistry, creating a mathematical model for an oscillating chemical system called the Belousov-Zhabotinsky, or BZ, reaction, in which a certain chemical solution changes from blue to red and back again and spontaneously forms spatial patterns. She became an expert in oscillating systems, which happen to be rampant in neuroscience. Walking, chewing, swimming, and many other motions rely on oscillating brain waves, and neuroscientists started asking Kopell to create mathematical models for their experiments.
“The brain produces all of these rhythms that are associated with cognition, that seem to have nothing to do with what you actually do with any muscle,” she says. She suspects that a malfunction in these rhythms may be responsible for cognitive problems associated with many neurological diseases, like Parkinson’s. The idea is controversial. “There are still a few people who claim that these rhythms are like the sound of the exhaust in a car: they have nothing to do with what the car is actually doing, they just happen to be around,” she says. “Many of the rest of us think that these rhythms are actually critical parts of the computations that the brain makes.”
Kopell is working with BU postdoctoral fellow Sujith Vijayan on the disruption of sleep by alpha waves in patients with fibromyalgia, a syndrome of chronic widespread body pain. In addition, she and another team, which includes Michelle McCarthy, a CAS research assistant professor of mathematics and statistics, are investigating how the brain in Parkinson’s patients produces pathological rhythms and how treatments such as deep brain stimulation help to restore function.
She is also continuing her work on anesthesia. Study coauthor Brown’s group has started to investigate other anesthetics and plans to study the effects on elderly patients, who are much more sensitive to the drugs. This can lead to anesthesia that is too deep, causing permanent dementia.
Kopell will create mathematical models of the effects of the various anesthetics in the young brain and the aging brain, with the hope of understanding what makes the elderly so much more sensitive.



































Related Stories
Unexpected Awakenings
Nancy Kopell’s research could help prevent people from waking up under anesthesia
Kopell Wins Israeli Nonprofit’s Mathematical Neuroscience Prize
Honors research in brain dynamics underlying cognitive function
Kopell Wins Society for Neuroscience Swartz Prize
Recognized for pioneering role in computational brain studies
Post Your Comment