Systematic Review of the Effects of Exercise and Physical Activity on Psychological and Quality of Life Outcomes for Individuals with Multiple Sclerosis, 1996–2011
Systematic Review of the Effects of Exercise and Physical Activity on Psychological and Quality of Life Outcomes for Individuals with Multiple Sclerosis, 1996–2011
Suggested Citation: Anthony, W., & Gidugu, V. (2012). Systematic Review of the Effects of Exercise and Physical Activity on Psychological and Quality of Life Outcomes for Individuals with Multiple Sclerosis, 1996-2011. Boston: Boston University, Sargent College, Center for Psychiatric Rehabilitation. https://www.bu.edu/drrk/research-syntheses/multiple-sclerosis/effects-of-exercise/
Conducted by the Center for Psychiatric Rehabilitation with support from the National Institute on Disability and Rehabilitation Research.
Table of Contents
Plain Language Summary
Contributors
Introduction
Background
Objective of the Systematic Review
Methods and Procedures
Results
Conclusions from Experimental Studies
Conclusions from Non-Experimental Studies
Acknowledgements and Statement Concerning Conflict of Interest
Appendix A: Table of All Studies Reviewed
Appendix B: Rating Scale for Rigor
Appendix C: Rating Scale for Meaning and Perceived Utility
Appendix D: References
Review was conducted using a system for rating the rigor and meaning of disability research (Farkas, Rogers, & Anthony, 2008). The first instrument in this system is: “Standards for Rating Program Evaluation, Policy or Survey Research, Pre-Post and Correlational Human Subjects Studies” (Rogers, Farkas, Anthony, & Kash, 2008) and “Standards for Rating the Meaning of Disability Research” (Farkas & Anthony, 2008). A full listing of contributors is contained in the section “Contributors.”
Plain language summary
Multiple sclerosis (MS) is an autoimmune disease in which the body’s own defense system attacks the fatty substance (myelin) that surrounds and protects the nerve fibers in the central nervous system. The nerve fibers themselves can also be damaged. The damaged myelin forms scar tissue (sclerosis), which gives the disease its name. When any part of the myelin sheath or nerve fiber is damaged or destroyed, nerve impulses traveling to and from the brain and spinal cord are distorted or interrupted, producing the variety of symptoms that can occur in individuals with multiple sclerosis.
There are approximately 400,000 people with MS in the United States and about 2 million people worldwide. MS is more common in women than men, more common in the northern latitudes, and typically is diagnosed in people between 20 and 50 years of age. The resulting disability from MS is unpredictable and can progress to severe limitations in functioning. MS presents with significant variability over time in the intensity and variety of symptoms, which can include limitations in muscular strength, balance, coordination, energy, bladder and bowel control, and sexual function, as well as deficits in cognition and mood.
The objective of this review is to determine whether exercise interventions and physical activity have an effect on psychological factors and quality of life among individuals with multiple sclerosis. Results of this systematic review provide some evidence to indicate that participation in exercise can improve various psychological and social dimensions of self-reported quality of life and/or mood for individuals with mild to moderate MS. No body of evidence exists for the psychological effects of exercise on people with severe MS because no studies have been conducted on individuals with more severe symptoms and illness. Similarly, there is no body of evidence at present that indicates that exercise interventions can affect cognitive functioning. Furthermore, no particular exercise intervention program appears to outperform any other. That is, whether the exercise intervention was resistance training or a particular type of aerobic training did not seem to matter. The reason exercise interventions affect mood and quality of life are unknown and may be partially due to the social support that can be available during an exercise intervention. We also found evidence linking increased physical activity with higher quality of life, less depression, and greater self-esteem. It may be that depression and fatigue are important factors in the levels of physical activity that people engage in, rather than simply the pain and symptoms related to MS.
More study is needed both in terms of determining effective exercise interventions and understanding the complex relationships that exist between physical activity and psychological well-being, pain, symptoms, and fatigue.
Contributors
Lead Reviewer:
William Anthony, Ph.D.,
Executive Director the Center for Psychiatric Rehabilitation and Professor,
Boston University, Sargent College of Health and Rehabilitation Sciences
Study Group:
William Anthony
Vasudha Gidugu
E. Sally Rogers
Mihoko Maru
Lauren Mizock
Marianne Farkas
940 Commonwealth Avenue West
Boston, MA 02215
Additional review and scientific consultation was received from Charles Bombardier, Ph.D., University of Washington Multiple Sclerosis Rehabilitation Research and Training Center.
For additional information, contact E. Sally Rogers at erogers@bu.edu.
Introduction
As described by the National Multiple Sclerosis Society, multiple sclerosis (MS) is an autoimmune disease in which the body’s defense system attacks the fatty substance (myelin) that surrounds and protects the nerve fibers in the central nervous system. The nerve fibers themselves can also be damaged. The damaged myelin forms scar tissue (sclerosis), which gives the disease its name. When any part of the myelin sheath or nerve fiber is damaged or destroyed, nerve impulses traveling to and from the brain and spinal cord are distorted or interrupted, producing the variety of symptoms that can occur (National Multiple Sclerosis Society [NMSS], 2011).
There are approximately 400,000 people with MS in the United States and about two million people worldwide. MS is more common in women than men, more common in the northern latitudes, and typically is diagnosed in people between 20 and 50 years of age (NMSS, 2011). The resulting disability from MS is unpredictable. MS can progress to severe limitations in functioning. MS presents with significant variability over time in the intensity and variety of symptoms, which can include limitations in muscle strength; balance; coordination; energy; and bladder, bowel, and sexual function; as well as cognitive deficits and mood disturbance. Studies have shown that in addition to reduced strength, balance, and coordination, individuals with MS have reduced levels of endurance and cardiorespiratory fitness (White & Dressendorfer, 2004), which can be affected by exercise and physical activity.
Although a variety of medical and pharmacologic interventions have been tested for individuals with MS to reduce symptomatology, we were particularly interested in the role of exercise and physical activity in improving quality of life outcomes among individuals with MS. Thus, the purpose of this systematic review was to examine effectiveness of exercise interventions and physical activity on psychological and social factors among individuals with MS.
Background
Until the latter part of the 20th century, exercise was seen as detrimental to the course of MS and, not surprisingly, people with MS limited their physical activity. Despite the absence of empirical evidence, physicians advised their patients with MS to avoid physical activity in order to help minimize the risk of exacerbation and fatigue (Sutherland & Andersen, 2001). Conventional thinking at the time was that physical activity might cause an exacerbation of symptoms and increased disability (Gallien et al., 2007). Because the elevated body temperature brought about by exercise could cause a temporary worsening of MS symptoms, there was a concern that exercise and physical activity would have permanent deleterious effects on symptoms (Heesen, Romberg, Gold, & Schulz, 2006). This medical advice about the effects of exercise was contradictory to the advice given to healthy individuals about the value of exercise.
In 1996, Petajan and colleagues published the first randomized trial to demonstrate that exercise could have positive effects on physical functioning without any negative effects on MS symptoms or level of disability. Since that time a Cochrane collaboration review (Rietberg, Brooks, Uitdehaag, & Kwakkel, 2004) of nine randomized controlled trials (RCTs) on exercise therapy for people with MS concluded that there was strong evidence supporting exercise therapy when compared to no exercise therapy with respect to improvements in muscle function and mobility, and these same studies reported no deleterious effects of exercise. For the Cochrane review, exercise therapy was defined as “a series of movements with the aim of training or developing the body by a routine practice or as a physical training to promote good physical health” (Webster’s New World Dictionary, 1982). In 2009 a meta-analytic review of RCTs and pre-post studies also reported positive results (Snook & Motl, 2009). From a review of 22 studies, the authors concluded that, “the cumulative evidence supports that exercise training is associated with a small improvement in walking ability among individuals with multiple sclerosis.”
Based on this research examining exercise and MS, the medical community now views exercise as an important part of a comprehensive approach to treatment that results in positive and no negative effects. As evidenced by the research we examined for this review, the role of exercise in the lives of individuals with MS continues to engage the attention of the medical and healthcare communities.
Impact of exercise on psychological factors
During this same period, several studies appeared that suggested that exercise for people with MS might also have a beneficial effect on psychological as well as physical factors (Brown & Kraft, 2005). The 2004 Cochrane review, although primarily focused on the impact of exercise on physical functioning, also concluded that there was moderate evidence for the effect of exercise on improving mood (Rietberg et al., 2004). Such findings were of interest in the field of MS because of the known presence of difficulties in psychological functioning among people with MS. For example, in a population-based study of the prevalence of major depression in MS in Canada, researchers found that 25.7% of their sample of adults reported major depression, significantly higher than the general population (Patten, Beck, Williams, Barbui, & Metz, 2003). Researchers found an increased incidence of suicidal ideation among a sample of veterans with MS—fully 29% of the sample expressed suicidal ideation in a mail survey (Turner, Williams, Bowen, Kivlahan, & Haselkorn, 2006). Similarly, cognitive dysfunction (e.g., in memory, information processing speed, executive function) is common in around 40–70% of people with MS (Brown & Kraft, 2005; Thompson, Toosy, & Ciccarelli, 2010). Development of measures of affective and cognitive dysfunction that are used in studies of exercise and MS has largely built from existing psychological measures in other fields. Some examples of measures used in MS exercise studies of psychological functioning include the Profile of Mood States (Petajan et al., 1996), Beck Depression Inventory (Stroud & Minahan, 2009); those for cognitive functioning include the Wechsler Memory scales III Logical Memory (Oken et al., 2004).
Impact of exercise on quality of life
The “quality of life” construct entered the American vocabulary in the mid-20th century (Ferrans & Powers, 1985). The use of quality of life measures in MS research did not occur until the 1990s (Nortvedt & Riise, 2003). Since that time, researchers have attempted to arrive at an accepted definition and method of measurement. Quality of life can be described as a person’s assessment of how well one is living across a variety of domains (Motl & Gosney, 2008), in essence reflecting a global satisfaction with life (Motl et al., 2008). Quality of life among people with MS is poorer in comparison to both healthy populations (Hart, Fonareva, Merluzzi, & Mohr, 2005) and to people with other chronic illnesses (Rudick, Miller, Clough, Gragg, & Farmer, 1992). In 2008, Motl and Gosney used meta-analytic procedures in a review of the effect of exercise interventions on quality of life, and reported that exercise is associated with small improvements in quality of life.
In studies of MS, quality of life sometimes referred to a person’s perception of physical health–related dimensions, such as a person’s subjective estimates of fatigue, pain, general health, mobility impairment, and the effect of these physical health dimensions on functioning. In some early studies, psychological factors were often of less interest in defining quality of life (Hart et al., 2005). For example, in the Motl and Gosney review, fatigue was included as a measure of quality of life (2008). In this review an attempt has been made to focus only on studies reporting on quality of life measures from which an estimate of psychosocial quality of life can be obtained, separate from physical health quality of life estimates. The Multiple Sclerosis Impact Scale (MSIS-29) is an example of several scales that measure quality of life with respect to both the physical and psychological impact of multiple sclerosis (Hobart, Lamping, Fitzpatrick, Riazi, & Thompson, 2001). Another example is the mental component scale (as opposed to the physical component scale) of the Short Form Health Survey (SF-36) questionnaire (Dalgas et al., 2010). Fatigue, pain, and other physical measures can certainly affect quality of life. However, such dimensions are excluded from this review as we targeted only psychological factors.
Some studies by MS researchers have measured quality of life using scales developed for the general population, such as the SF-36 (Ware et al., 1993), whereas other researchers have used quality of life instruments that were developed specifically for people with MS (Motl & Gosney, 2008). The Multiple Sclerosis Quality of Life Scale-54 (MSQOL-54) is a composite measure comprising the SF-36 as well as disease-specific scales that measure mental health and physical dimensions underlying quality of life (Vickrey, Hays, Harooni, Myers, & Ellison, 1995). Nortvedt and Riise (2003) reviewed 33 different quality of life–related instruments used in studies of MS; 10 of these instruments were specifically designed for MS. As this review is not a review of quality of life instruments per se, no attempt was made to review separately the impact of exercise therapy on disease-specific and general quality of life measures (Motl et al., 2008). Studies are included that use disease-specific and/or general quality of life instruments.
Objective of the Systematic Review
The aim of this review is to determine whether exercise interventions and physical activity are effective for individuals with MS in terms of improving psychological factors and quality of life (QOL).
Methods and Procedures
The study group received assistance and guidance on the search terms and procedures from the research director of the National Multiple Sclerosis Society. We searched for any study or article that included an exercise intervention or an intervention focusing on improving physical fitness and well-being, and that also measured psychological, social, or quality of life outcomes. The alternate terms used for exercise were exercise therapy and exercise movement techniques. Exercise was defined as “a series of movements with the aim of training or developing the body by a routine practice or as a physical training to promote good physical health.” This is same as the definition of exercise therapy used by Rietberg et al. (2004) in their review, “Exercise Therapy for Multiple Sclerosis.” We excluded studies using only physical therapy. We included both efficacy and effectiveness studies, as well as empirical studies of the association between measures of physical activity and measures of psychological functioning, social functioning, and quality of life.
We did not exclude by any particular MS subpopulation, however, we note that the preponderance of studies are focused on individuals with moderate, not severe, MS. Many of the samples lack ethnic diversity, and many have a preponderance of women, which may reflect the overall demographics of individuals with MS.
We included studies with a wide range of designs: randomized controlled trials, quasi-experimental trials, prospective cohort studies, correlational studies, and survey research.
The final search terms used were
- affective states,
- affect,
- mood,
- depression,
- well-being,
- psychological status,
- psychiatric status,
- mental health,
- mental status,
- mental health status,
- anxiety,
- psychological symptoms,
- psychiatric symptoms,
- emotional functioning,
- emotional well-being, and
- quality of life.
In addition, we used the following terms as a way of insuring a comprehensive search, although these outcomes were not of primary interest:
- neuropsychological symptoms,
- cognition, and
- cognitive functioning.
Databases searched included: PubMed, Medline, Web of Science, Psych Info, Google Scholar, CINAHL, and Cochrane Collaboration. We examined the citations contained in each article for additional potential articles and reports to review, performing a legacy search, in which we examined all citations in the located studies and articles.
One senior research assistant was responsible for querying the databases and locating articles under the direction of the lead reviewer, who scanned the titles of articles for relevance to the objective of the review. If the title appeared relevant, the abstract was reviewed, and if it was deemed likely to meet inclusion criteria, the article was obtained. A checklist of inclusion/exclusion criteria was completed for each article to facilitate tracking of articles screened. In some cases, once the article was reviewed, it was clear that the inclusion criteria were not met. Occasionally, one or more members of the study group had to be consulted to make a determination about including or excluding an article. We did not search for or include conference proceedings.
Based on this process, a total of 128 articles were located and 37 selected to be rated for rigor, which determined their inclusion in synthesis and being rated for meaning. The remaining 91 articles did not meet the criteria for inclusion in rating. Of these, 59 were excluded because they did not address the content areas of interest, in that they were either not specific to MS, were not related to exercise, did not report on any psychological or QOL factors, or contained only physiological assessments. One article was excluded because there was no description of the control intervention. Four articles were excluded because they were either qualitative or descriptive but did not attempt to examine the effect of exercise on psychological or quality of life outcomes. Eleven other articles were excluded because they did not focus on exercise interventions. These included articles related to QOL measures, scale development, hypothesis generation, editorials, or commentary. In addition we excluded 16 review articles. Some of the articles that were excluded for this review were used as background material (as noted above). Figure 1 outlines the information about articles identified and included.
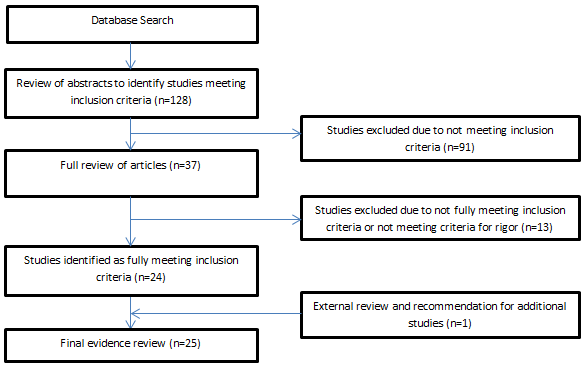
Figure 1 shows that of the 37 studies remaining to be reviewed, 13 were excluded from the narrative synthesis after being rated for quality because methodology scores were low enough that the conclusions could not be considered robust or valid. (See the section below and Appendix B for additional detail about the items used to rate quality.) Issues such as a very small n (fewer than 10), very poor research design with major threats to internal validity, questionable measurement, as well as very large attrition of study subjects (with no explanation of how they were handled in the analyses) were all reasons for exclusion. Note, however, that the excluded articles appear in the reference list preceded by a “*” so that the reader can examine all studies in the original pool.
Once a complete list of articles for review was compiled, that list was sent to several MS experts and scientists. We asked those experts to review the list to ensure that no relevant article or report was omitted. This step yielded one new citation appropriate for review, an unpublished manuscript. This manuscript was rated for rigor and met the standards for inclusion. With this addition the total number of articles rated for rigor was 38. Note that only those articles that were included in the synthesis after rigor ratings were also rated for meaning.
The 25 articles reviewed and included in the narrative synthesis were classified as primarily randomized controlled trials (n = 14), quasi-experimental trials (n = 3), prospective cohort studies (n = 3), and cross-sectional/correlational survey research (n = 5). (See Appendix A, which lists all studies reviewed by type of study and summarizes their purposes and findings.)
Ratings of the Quality of the Research
The quality of the research for this systematic review was determined by examining both the rigor (traditional indicators of the quality and appropriateness of the methodology) and the perceived meaning of the research (that is, the perceived utility and meaning the research has for the field, for policy makers and providers, and for consumers and family members).
Quality of the research was determined using a 21-item scale (see Appendix B for the Rigor Scale) that examined the quality of the rationale for the study, the research design used, the data collection and analysis methods, the explanation and interpretation of findings, and the discussion of the results. Items were rated on a 4-point scale indicating whether the researchers addressed the item Not at all, Minimally, Somewhat, or Definitely. The review team developed the 21 items of the Rigor Scale by examining the standards and items put forth by other scientific bodies, including the National Research Council, the Agency for Health Care Quality and Research (West, King, Carey et al, 2002), and CONSORT (Moher, Schulz, & Altman, 2001), as well as numerous other documents describing approaches to rating the quality of research. We borrowed heavily from these documents and other information about the quality of research. Because we were examining data beyond randomized trials, we could not simply use the CONSORT standards; we had to construct items that would be useful to measure designs that are generally considered less rigorous, such as quasi-experimental designs.
The team also developed a measure of perceived utility of the research. That scale consisted of 19 dichotomously rated items (Yes/No) designed to determine the involvement of individuals with MS in the conceptualization, conduct, or interpretation of study findings; collection and presentation of data from the study that would be meaningful to individuals with disabilities; and the support available to implement the intervention being studied in routine service settings.
As noted above, of the 38 articles rated for rigor (see Appendix B for Rigor Scale), 13 were excluded from the narrative synthesis based upon their poor scores in the methodology section. Studies that employed weak designs for the questions they were addressing or had severe threats to internal validity were excluded. We used a score of 2.0 or below as a cutoff for the major methodology item—The study/research uses rigorous or sound research methods that allow the questions of interest to be addressed. Any study with a score of 2.0 or below on this item was excluded from the narrative synthesis because the findings could not be assumed to be valid given the low methodology rating.
Time Period of the Studies and Research Covered
We considered any study published in the 15 years prior to the date of the systematic review (1996–2011). The study team decided on a 15-year review period because it coincided with the first and seminal study by Petajan and colleagues (1996), which examined the role of exercise and its effect on quality of life among patients with MS.
Training of Reviewers
A total of four raters were used for this systematic review. All were individuals affiliated with the Center for Psychiatric Rehabilitation, including research staff, the executive director (the lead reviewer), and post-doctoral fellows in residence. The articles were evenly divided among raters. The study consultant, Dr. Bombardier, is affiliated with the University of Washington Multiple Sclerosis Rehabilitation Research and Training Center.
Each rater was knowledgeable prior to the beginning of the systematic review about research methods, so their training focused on what kind of evidence for research quality might be encountered in published articles and what would be an acceptable indicator that quality had been achieved for each of the four points on the rating scale. All individuals were trained in the use of the rating scales by reviewing each item of the scale and discussing the meaning of the item and the evidence that could be considered for each indicator. Research articles were used as training devices by having each rater independently review articles and then discuss their ratings with the review group members until acceptable inter-rater agreement was achieved. We examined inter-rater reliability by bifurcating the agreement scale (into Acceptable or Unacceptable quality) and then comparing reviewers’ ratings to the “expert” or “gold standard” reviewer. Results for the 20 items of each of the practice articles suggested very good inter-rater reliability: 100% agreement on 30 out of 40 items (20 items for each of the two articles); 80% agreement on 6 items; 60% agreement on two items, and 40% agreement on a final two items. Throughout the rating process, when a rater had difficulty reaching a decision about a rating of quality, consensus ratings were used among members of the study group as a way of ensuring the most accurate and reliable final ratings.
Results
Results of the ratings of rigor and meaning
The results suggested that the highest average scores received for rigor among the rated studies were in the presentation of the findings (that is, the findings were presented logically and flowed from the results); the introduction to the problem and the rationale for the study; and the comparison of the findings in the discussion section to other important studies and findings (average scores of 3.84, 3.64, and 3.76, respectively). The methodology and the discussion sections resulted in the lowest ratings with certain average methods ratings being rated just barely adequate (i.e., below a 3.0 score). In particular, the description of the handling of the data and the handling of missing data, the description of the control or comparison conditions, and descriptions related to the generalizability of the findings received among the lowest scores (i.e., 2.64, 2.75, and 2.20, respectively).
Because we are using an innovative approach to assessing perceived utility for the studies reviewed, ratings of meaning (see Appendix C for Meaning Scale) were not used to exclude articles from the narrative synthesis, but rather to get a preliminary sense of whether and how the meaning of studies would be rated using this newly developed scale. We found that there was very little reported involvement of consumers (4% to 12% of the studies reviewed) in the design, implementation or review of research studies. We also rated whether information was collected and presented in the article using the World Health Organization framework for reporting functioning, disability, and health. Ratings in that section suggested that data were routinely presented on indicators of health (100% of the time), but much less frequently in terms of tasks or activities performed, role functioning, or on environmental factors related to activity and participation (60%, 16%, and 4% of the time, respectively).
We also rated whether the authors of the article articulated implications of the research for various levels of stakeholders—including policy makers, service providers, practitioners, consumers, and families—and found very few such discussions. Implications for policy/systems development were never mentioned, implications for programs and services were mentioned 52% of the time, implications for the daily life of individuals with disabilities were mentioned 62% of the time, and implications for provider practice were described 28% of the time. Rarely do the authors discuss implications for family members of individuals with MS (4% of the time), and there was no discussion at all for minority or underserved individuals with MS.
The final section of the Meaning Scale asks whether information, tools, or other supports are available to put the intervention or information studied to use in the field. We found that in a small number of studies, the authors spelled out values underlying the intervention or service being studied (20%), but other supports for implementing interventions were virtually never present in the article (that is, supports such as materials or tools for implementation, help with translating the findings into practice, or support for underserved populations).
Results from Experimental Studies of Exercise Interventions
In 1996, at a time when exercise was believed to be detrimental to individuals with MS, Petajan and colleagues conducted a randomized controlled trial to determine the effects of exercise on fitness and other areas affected by MS such as fatigue, functioning, and mood. Fifty-four patients with MS were randomized to an exercise group or a non-exercise control group. Participants were selected based on a clinically confirmed diagnosis of MS, Expanded Disability Severity Scale (EDSS) scores of 6 or less and no history of cardiovascular, respiratory, orthopedic, metabolic, or other medical conditions. None of the subjects had participated in any form of regular physical activity in the past 6 months. The exercise intervention consisted of three 40-minute sessions per week of combined arm and leg ergometry for 15 weeks. Assessments included neurological assessment of MS by a blinded neurologist using Kurtzke’s Functional System Scale, EDSS, and the Incapacity Status Scale; physiological measurements of exercise capacity using Graded Exercise Test (GET), strength, body composition analysis, and blood lipids; psychological assessments of mood using Profile of Mood States (POMS); health status using Sickness Impact Profile (SIP); and fatigue using Fatigue Severity Scale (FSS). Of the 54 participants originally selected, 6 were excluded for reasons unrelated to the study and MS, and 2 were excluded secondary to an MS exacerbation. Data from 46 participants were used for analysis. The exercise group had significantly greater improvement in aerobic capacity, and in upper and lower extremity strength when compared to the non-exercise group over time. There was significant improvement in depression and anger in the exercise group only at 5 and 10 weeks, but there were no lasting significant changes in mood states in either group at 15 weeks. Differences in POMS scores between the groups were not presented. The exercise group had significant improvements in the physical dimension of the SIP scores; there were no significant differences between groups or significant changes over time in the psychosocial dimension in either group, although the exercise group had significant improvement at Week 10 and in recreation and pastimes components at Week 15. Based on these findings, the authors recommended that individuals with MS be encouraged to engage in regular aerobic exercise. The exercise intervention was closely associated with socialization, which the authors note makes it difficult to separate the effects of fitness improvements from those of enhanced social interactions.
Solari and colleagues (1999) examined the efficacy of an inpatient physical rehabilitation program on individuals using a randomized design. A total of n = 304 MS patients were recruited and n = 50 enrolled in the study. The authors imposed very lengthy inclusion and exclusion criteria. Participants were included who had clinically definite MS, an Expanded Disability Status Scale of between 3.0 and 6.5, no significant cognitive impairment, and who were not in an exacerbation of the illness. They were excluded if they had a history of cardiovascular, respiratory, orthopedic, psychiatric, or medical conditions precluding participation, including treatment with several specified drugs. All consecutively hospitalized patients and outpatients during the study period were considered for inclusion in the study, and after the criteria were applied, n = 27 were randomized to the treatment group and n = 23 to the control group. Individuals were assessed using a neurological exam (by a nontreating physician), Hauser’s Ambulation Index, the Functional Independence Measure, and the Hamilton Rating Scale for Depression. Health quality of life was assessed using the SF-36. The intervention lasted for 3 weeks and consisted of twice daily exercise periods (a total of 15 sessions), each lasting 45 minutes. Patients were instructed to perform exercises at home as well. Control participants received a 1-day session of instruction from a physiotherapist, were instructed to perform home exercises, and were also trained in mobility aids and orthoses. A total of five individuals withdrew before the end of the 15-week treatment and observation period. Researchers used an intent-to-treat (ITT) analysis. Improvements were seen in some physical domains. On the SF-36, all scales improved in the experimental group, but there was no statistically significant difference between the experimental and control groups except on the mental health composite index. The study may have been underpowered with respect to the SF-36 because power calculations were not conducted on this measure. The generalizability of the study also appears limited because of the very stringent exclusion criteria.
In a 2001 randomized trial, Sutherland, Anderson, and Stoove examined the effect of an exercise intervention using the rationale that a sedentary lifestyle can dramatically reduce quality of life, increase depressed mood, diminish sociability, and lead to a decline in general well-being. The authors recruited 22 participants through the Multiple Sclerosis Society of Victoria, Australia, matched those individuals for age and gender, and randomly assigned them to the experimental water aerobics group (n = 11) or the control group of no exercise (n = 11). They examined the influence of aerobic exercise on psychological well-being and health-related quality of life. They used the Multiple Sclerosis Quality of Life-54 measure, the Profile of Mood States, and the Multidimensional Scale of Perceived Social Support. The intervention was designed to be 10 weeks long, 3 times per week. The authors controlled for social support so that they could assess the unique effects of the exercise regimen apart from the social activities and support imparted by the exercise classes. They concluded that their structured 10-week aerobic/anaerobic exercise program had a positive effect on well-being and components of mood measured by POMS- including improvements in pain, tension, social and sexual functioning, vigor/fatigue, and energy even when controlling for social support. Observed changes in depression component of POMS were in the predicted direction but were not significant. The very small sample limits the study’s conclusions, as does the authors’ failure to describe the recruited and screened study participants.
Mostert and Kesselring (2002) conducted a randomized controlled trial to study the impact of short-term exercise on MS using a four-group design; two groups were composed of individuals with MS, and two were composed of “healthy persons.” Thirty-seven participants with MS from an inpatient rehabilitation program in Switzerland were randomized to either an exercise training (MS-ET) or nontraining group (MS-NI). Inclusion criteria for MS patients were: a confirmed diagnosis of clinical MS with any disease course; ability to pedal on a freestanding bicycle ergometer; and no history of cardiovascular, respiratory, orthopedic, or metabolic diseases or other medical conditions that would preclude participation in the exercise program. No patient had an exacerbation of MS during at least 2 months prior to the training. Of the 37 patients originally selected for the study, two were excluded because of changes during exercise in their electrocardiogram. Three patients of the exercise group quit the study directly after random assignment to the exercise group. Two suffered from elevated spasticity of the lower extremities after testing. In the non-exercise group, three patients had difficulty sustaining the intervention program; two others had symptom exacerbations. Data from the 26 remaining subjects were used for statistical analysis (exercise n = 13, non-exercise n = 13) and were compared to matched controls (matched on age, gender, and activity levels). The exercise training involved five 30-minute supervised training sessions per week. Patients in the non-exercise group participated in physical therapy within the rehabilitation program but agreed not to increase their physical activity level. In addition to physical outcomes, questionnaires to measure health perception (SF-36), and fatigue (Fatigue Severity Scale) were administered to all patients at baseline and at the end of 4 weeks of rehabilitation. The study found that the maximal aerobic capacity of MS subjects was markedly lower than that of matched healthy controls and did not change in the MS exercise group. There was significant improvement on vitality and social functioning indexes of the SF-36 for the MS exercise group. There was no significant change in fatigue scores but a tendency for reduction was noted in the MS exercise group. The major limitation affecting this study was low adherence to the intervention. The authors note the importance of creating motivation for engaging in exercise.
Oken and his colleagues (2004), arguing that yoga may have a beneficial effect on multiple sclerosis, performed a randomized clinical trial examining the effect of a structured and tailored yoga intervention versus an aerobic exercise intervention or a wait-list control group. They recruited and screened n = 129 individuals and randomized n = 69 to one of the three groups (n = 21 to aerobic exercise; n = 26 to the yoga group; n = 22 to the wait-list control). The two exercise interventions were designed to be 26 weeks in duration, and the authors measured how intensively participants engaged in the respective interventions. Overall, attendance at weekly classes (aerobic and yoga) was 65%, and home exercise (which participants were encouraged to do) was 45%. The authors examined outcomes using a variety of measures, including the SF-36, the Profile of Moods States, and the CES-D scale for depression. They also examined several cognitive outcomes, alertness, quality of life, fatigue, and additional physical outcomes. They found no significant effect of group assignment on any of the cognitive function or alertness measures. The two exercise groups were significantly better than the wait-list control on several self-report measures, including the SF-36 Vitality measure and the Multi-Dimensional Fatigue Inventory (MFI). The authors note that the improvement in fatigue was partially independent of depression because there was not a significant effect of the interventions on depression. Some limitations of this study include the fact that, as the authors state, it was underpowered to test the effects of the intervention on cognitive outcomes; and the study included almost exclusively women. A large number of outcome tests were conducted because of the large number of variables the authors were exploring, creating the possibility of tests yielding spurious findings. Further, the authors do not report the results of analyses on the groups as assigned (i.e., intention-to-treat [ITT] analyses).
Schulz and colleagues (2004) studied the immune-endocrine and muscle coordination factors that mediate the relationship between exercise and quality of life for individuals with MS. The study used a randomized control trial design in two parts. Individuals recruited to the study were excluded if they failed an exercise endurance test; n = 18 were so excluded. Participants were then randomly assigned to an 8-week bicycling training group or a wait-list control group. Due to the small sample size in the initial recruitment phase of the study, a second study was conducted to focus on coordination factors; it was also offered to individuals who had been originally excluded from the study. Therefore, 11 of the excluded participants were included in the second phase of the study, which focused on coordinative function. Study 1 focused on immune-endocrine factors (n = 15 exercise, n = 13 control) and Study 2 focused on muscle coordination function (n = 23 exercise, n = 16 control). Quality of life was measured using the Hamburg Quality of Life Questionnaire in Multiple Sclerosis (HAQUAMS) and the SF-36. Affect was measured using the Profile of Mood States and the Hospital Anxiety and Depression Scale. Fatigue was measured using the Fatigue Impact Scale (FIS). Self-efficacy was measured using the MS Self-Efficacy Scale. Study 2 findings showed an improvement in muscle coordination and improvement in disease-specific quality of life. However, no significant differences were found on the SF-36 measure of quality of life, the Profile of Mood States scale, the FIS, self-efficacy scale, or Hospital Anxiety and Depression Scale. These results suggest that a relatively brief exercise intervention can improve quality of life for individuals with MS. Limitations included small sample size and reduced power. Generalizability was also limited by the focus on individuals with relapsing-remitting MS. Lastly, one third of the MS patients had to be withdrawn because they were not able to finish the tests properly, which also affected the power of the study.
Romberg, Virtanen, and Ruutiainen (2005) conducted a randomized controlled trial to examine the impact of long-term exercise on the quality of life and functional impairment of individuals with relapsing-remitting MS. Participants were randomly assigned to a 6-month progressive exercise group (n = 47) or the control group (n = 48). Depression, functioning level (Multiple Sclerosis Functional Composite [MSFC]), quality of life (MS Quality of Life Scale-54), functional independence (Functional Independence Measure), depression (Center for Epidemiologic Studies Depression Scale), and disability status (Expanded Disability Status Scale [EDSS]) were assessed at baseline and at 6 months. Results indicated improvements for the exercise group in the area of leg function and movement. No improvements were found on depression, functional independence, quality of life, or disability status. Unique aspects of the intervention may account for these findings, in that participants exercised alone for 23 weeks, whereas in another study that had significant findings, participants exercised in small groups for 15 weeks. It is possible that such an intervention provides social support that may in turn affect quality of life. It is also possible that this measure of quality of life was not as well suited to detecting changes in quality of life in the context of the present study. Limitations included potential practice effects of re-administering the Multiple Sclerosis Functional Composite (MSFC) and inability to blind participants to the assigned condition (a potential limitation in most, if not all, such studies). Another limitation was randomization prior to clarifying eligibility for the study.
McAuley and colleagues in 2007 conducted a randomized controlled trial comparing the effects of an self- efficacy enhancement intervention and a control (standard care) condition on exercise adherence, well-being, and affective responses to exercise. The sample was drawn from the nearby community through recruitment at the local National Multiple Sclerosis Society, media advertisements, and by contacting individuals from previous studies of MS. Eligibility criteria included having a definite diagnosis of MS, being ambulatory with minimal assistance, and being sedentary. A total of N = 26 were randomized to one of the two conditions, with half (n = 13) to the efficacy enhancement condition and the other half to standard care. Data were collected on self-efficacy (Exercise Self-Efficacy), well-being (Satisfaction with Life Scale and Short Form Survey (SF-12), enjoyment, affective responses (Feeling Scale), and perceived exertion (Borg’s 15-point RPE scale). Exercise logs were completed by the exercise leader at each exercise session to measure exercise adherence. The experimental intervention consisted of the provision of efficacy-based information about physical activity, such as the importance of realistic, challenging, and attainable goals. Lectures with discussion, homework assignments, and buddy groups for social support were also part of the experimental condition. The standard care condition workshops focused on presentation and discussions of general health-related topics, such as benefits associated with increased physical activity. Both groups participated in a 3-month physical activity program, during which they met with a trained exercise leader for 1-hour sessions three times a week. A moderate effect on exercise adherence (demonstrated by greater attendance and longer exercise time) was observed in the efficacy-enhancement intervention group. Statistically significant effects were seen in this group on affective response (i.e., feeling better after exercise). The intervention group also maintained levels of satisfaction with life over the 3-month period, although the same outcome declined in the standard care group. Perceived physical health remained mostly stable across time, however, perceived mental health declined in both groups. Furthermore, self-efficacy and one of the affective response outcomes (i.e., enjoyment reported after exercise) were also positively correlated with exercise adherence. The small sample size and its composition of mainly of females are the primary limitations of the study.
Dettmers, Sulzmann, Ruchay-Plossl, Gutler, and Vieten in 2009 sought to examine the impact of endurance training on MS patients with low to moderate levels of disability who complained of fatigue. Endurance training was compared to an intervention that included stretching, balance training, and coordination. Thirty MS patients were randomized to either one of the interventions, with 15 participants in each group. Both interventions were delivered as add-ons to inpatient treatment, and patients receiving either intervention participated in thrice weekly sessions of 45 minutes duration each for a period of 3 weeks. The primary outcome measure was walking distance. Other measures of change included fatigue using Modified Fatigue Impact Scale (MFIS) and Fatigue Scale for Motor and Cognition (FSMC), depression using Beck Depression Inventory (BDI), and quality of life using HAQUAMS. Improvements in depression and quality of life were noted only in single patients in the control group and not in the intervention group. The authors mention missing data at follow-up as a limitation, even though there were no systematic differences between those who returned questionnaires and those who did not.
In 2010, Ahmadi, Nikbakh, Arastoo, and Habibi sought to determine the impact of yoga on balance, speed, endurance in walking, fatigue, and quality of life in MS patients. Twenty-one women with MS were randomized to a yoga group (n = 11) or control group (n = 10). Yoga group subjects participated in thrice weekly Hatha yoga sessions of 60–70-minute duration over 8 weeks. Balance, walking speed, and endurance were all assessed. Fatigue was measured using the FSS and the MSQOL-54 was used to measure QOL. Improvements noted in the yoga group were significantly greater than the control group. Fatigue levels reduced significantly for this group and there were greater improvements in physical function, emotional well-being, and cognitive function, as well as physical and mental health composite scores.
A study by Dalgas et al. (2010) used a randomized controlled trial design to examine the effects of progressive resistance training to promote muscle strength and functional capacity on fatigue, depression, and quality of life for individuals with moderate severity MS. Exercisers (n = 16) completed a 12-week progressive resistance training program and were compared to non-exercisers (control group; n = 15). Resistance training was performed for the lower extremities twice weekly in the exercise group. The control group was instructed to perform their daily activity as per usual and were offered the same 12-week progressive resistance training program at the end of the study. The two groups were compared at baseline, end of the intervention, and at a 12-week follow-up point. Exercisers had been instructed to continue the progressive resistance training on their own during the 12-week follow-up period. Fatigue was measured using the Fatigue Severity Scale. Depression was measured using the Major Depression Inventory (Olsen, Jensen, Noerholm, Martiny, & Bech, 2003). Quality of life was measured using the Short Form Health Survey (SF-36), which generates physical and mental health composite scores. Disability status was measured with the Expanded Disability Status Scale. Results indicated improvements in fatigue, depression scores, and quality of life for the exercise group, which were maintained at the 12-week follow-up. The control group completed the exercise intervention at the end of the study, and the original results were partially reproduced in the control group with some improvement in fatigue, but no significant improvement in depression and quality of life scores. This finding suggests limitations due to power. Limitations to generalizability were observed given selection of relapse-remitting individuals with MS. Other threats to validity included potential confounding effects of social interaction in the exercise group as well as inability to blind participants to the group assignment.
Sabapathy, Minahan, Turner, and Broadley (2010) conducted a study using a cross-over design to compare adaptations in functional and quality of life following endurance and resistance-exercise training in people with multiple sclerosis. Twenty-one individuals with MS who could ambulate independently with or without the use of walking aide were recruited at local community health centers for the study. Individuals participated in both exercise interventions, each intervention program lasting 8 weeks. There was an 8-week “wash-out” period before the start of the second intervention. The order of the intervention was randomized using a coin toss. Five participants dropped out of the study, making the total sample size sixteen, with 12 females and 4 males. Disease impact (Multiple Sclerosis Impact Scale), depression (Beck Depression Inventory), fatigue impact (Modified Fatigue Impact Scale), and quality of life (Health Status Questionnaire Short Form-36; physical and mental components) were also assessed. Individuals were also asked to complete the Borg Category Ratio Scale immediately after the exercise session to rate the level of exertion. Eleven participants performed the resistance-exercise first. During the endurance-exercise training program, participants completed a set of six different exercises, whereas participants in the resistance-exercise training performed three upper body and three lower body exercises, one core-strength and one stability exercise. Pre- and post-training results showed that there were no differences between the two training programs in physical ability or other outcomes including disease impact, fatigue, depression, and quality of life. No changes were observed in the psychological scale of MSIS, cognitive scale of the MFIS, depression, or quality of life. Small sample size may have limited both power and generalizability. Furthermore, two of the four investigators (data collectors) were not blinded to the order in which the participants had completed the training programs. Other aspects of the design of the study (e.g., cross-over design, coin-toss method used for randomization) are also possible limitations to the study.
In 2010, Velikonja, Curie, Ozura, and Jazbec studied the effects of sports climbing and yoga on MS. They randomized 20 subjects with relapsing-remitting or progressive MS with EDSS score ≤ 6 to yoga or a sports climbing intervention. The two groups were compared in terms of the intervention’s impact on cognitive function, mood, and fatigue. Both programs were held once a week for 10 weeks, and subjects were asked to attend at least 9 of 10 sessions. Disease was assessed by a neurologist using EDSS, spasticity by a physiotherapist using Modified Ashworth Scale, and cognitive function using several standardized measures. Mood was evaluated using the Center for Epidemiologic Studies Depression Scale, and fatigue was evaluated using the Modified Fatigue Impact Scale. In terms of cognitive function, subjects in the yoga program showed significant improvement only in selective attention. Neither set of subjects showed significant changes on tests of executive function. Neither intervention had a significant impact on mood. Only the sports climbing group had a significant reduction in level of fatigue. This study was limited by a small sample size and the impact of level of MS on outcomes was difficult to specify due to the heterogeneity of the two study groups.
In order to address the gaps in treatment for major depressive disorder (MDD) among people with MS, Bombardier and colleagues in 2011 studied the potential of exercise as an alternative to more standard treatments such as antidepressants or cognitive behavior therapy (CBT). They examined the impact of an intervention to increase physical activity using a randomized design with a wait-list control group. The intervention involved telephone counseling based on motivational interviewing techniques to promote home-based physical activity. The intervention was delivered through an initial in-person session that was followed by seven scheduled telephone counseling calls (at Weeks 1, 2, 3, 4, 6, 8, and 10), each lasting about 30 minutes, and a final in-person session. In addition, treatment group participants were allowed self-initiated phone calls to counselors between scheduled sessions using a toll-free number. Individuals between 18 and 70 years of age with clinically confirmed MS, an EDSS score of 5.5 or less, significant depressive symptoms, and diagnosis of MDD who were currently sedentary were included. Individuals with conditions that made exercise unsafe based on Physical Activity Readiness Questionnaire (PAR-Q), had extreme heat intolerance or experienced the Uhtoff effect, had a self-reported diagnosis of schizophrenia, paranoid disorder, bipolar disorder, active suicidal ideation, current alcohol or drug dependence, or who were unable to complete forms independently were excluded. Ninety-two participants were randomized: 44 into the treatment condition and 48 as wait-list controls. Dropouts were greater in the control (19%) versus the treatment (5%) conditions. The primary hypothesis was that the intervention group would demonstrate a significantly greater response rate, that is, at least a 50% reduction in depression severity, compared to the control group. Secondary hypotheses were that the treatment group would demonstrate a significantly greater decrease on measures of depression severity and be less likely to meet criteria for MDD or dysthymia at follow-up compared to the control group. Assessment of outcome variables occurred at baseline, at 12 weeks post-randomization, and at 24 weeks post-randomization for maintenance of effects in treatment group. A blinded interviewer conducted the assessment. The measure used for primary outcome was Hamilton Rating Scale for Depression (HAM-D). Structured Clinical Interview for DSM-IV (SCID), Hopkins Symptom Checklist (SCL-20), and Positive and Negative Affect Scale (PANAS) were used as secondary outcome measures. The results of the primary outcome showed no significant difference in response rate (that is, at least a 50% reduction in HAM-D score from baseline to 12 weeks) or remission rate (12-week HAM-D less than 8) between the treatment group and control group. In contrast, examination of effects using the HAM-D as a continuous measure showed that the intervention group reported significantly lower post-treatment depression severity compared to controls. Both ITT and completers-only analyses were performed, and they yielded nearly identical results. The treatment group reported significantly greater physical activity at 12 weeks compared to controls, indicating that the relatively brief telephone counseling was effective in increasing physical activity. Based on the findings, the authors point out that the study demonstrates that the antidepressant effects of physical activity found among older adults and people with primary depression may apply to people who have major depression in the context of MS. The limitations that may have been associated with the primary outcome being nonsignificant include HAM-D score being analyzed as a categorical measure and 35–50% participants already being on antidepressant treatment, which could have limited the magnitude of change.
Results from Quasi-Experimental Studies of Exercise Interventions
On the premise that mechanisms influencing fatigue differ based on the therapeutic technique, Rasova and colleagues (2006) sought to examine the impact of different techniques on fatigue, depression, deconditioning, and cardiorespiratory fitness and muscle performance. One hundred and twelve patients participated in this study over a 2-year period. The patients were chosen from all consecutive outpatients with MS who attended the center during that time and who showed no progression of disease in the preceding 3 months, no exacerbation of MS in the last 28 days, and no acute manifestation of other disease or injury; who were able to move independently and walk at least 20 m with the help of crutches (Expanded Disability Status Scale (EDSS) 0-6.5); who were indicated as able; and who agreed to undergo the program. The participants were assigned to one of four groups: Group #1—neurophysiologically-based physiotherapy; Group #2—aerobic training; and Group #3—a combined program consisting of aerobic training and neurophysiologically based physiotherapy. These were compared to Group #4—the group of patients who did not change their habits. The participants were allocated to groups on the basis of “next one, next group,” based on availability of space in the group. The patients were therefore not randomized and baseline analyses suggested that the groups were not matched. In the groups of rehabilitated and nonrehabilitated patients, an independent therapist examined the measures of impairment, disability, handicap, and quality of life. Impairment was examined by means of the EDSS, fatigue by Modified Fatigue Impact Scale (MFIS), depression by Beck Depression Inventory (BDI), disability by Wade and Collin’s version of Barthel index (BI), handicap by Environment Status Scale (ESS) and quality of life by Multiple Sclerosis Quality of Life-54 (MSQOL). Each of the interventions was delivered through twice weekly sessions over a 2-month period. Ninety-five patients finished the study: 24 patients in Group #1, 36 in Group #2, 19 patients in Group #3, and 16 patients in Group #4. The reasons for noncompletion of the 17 participants who did not finish the study included MS relapse, other illnesses, and loss of motivation. The authors did not conduct intent-to-treat analyses. The amount of change in the treated groups differed significantly from the nontreated groups. Changes in specific parameters were analyzed within groups only. Among other changes, significant reduction in fatigue and depression were noted in all three intervention groups; improvements in neurological impairment were noted only in Groups 1 and 3. Baseline differences in disability and impairment levels constitute the major limitation of this study.
McCullagh, Fitzgerald, Murphy, and Cooke (2008) performed a pilot study to examine the short- and long-term effects of exercise on quality of life and fatigue in people with MS using a randomized design. Individuals with a definite diagnosis of MS who were independently mobile without the use of aids, able to participate in the exercise intervention, and who were able to exercise independently at home were eligible to participate in the study. Those who had a relapse in the last 3 months, had a history of cardiac conditions, or a cognitive/psychological condition that would limit them from participating in the intervention were excluded from the study. Seventy-two were found eligible, of which 30 were recruited and randomized either to the exercise group (n = 17) or the control group (n = 13). All participants were assessed at baseline, at 3 months, and at 6 months for quality of life (Functional Assessment of Multiple Sclerosis scale [FAMS], and the Multiple Sclerosis Impact Scale-29 [MSIS-29]), fatigue (Modified Fatigue Impact Scale) and exercise capacity. The FAMS scale contains six subscales measuring mobility, symptoms, emotional well-being, general contentment, thinking/fatigue, and family/social well-being. The MSIS-29 consists of 20 physical and nine psychological dimensions. Exercise capacity was measured using a graded exercise test. The intervention group participated in exercise classes that were held twice weekly for 12 weeks. Participants also completed a self-selected home exercise program. Control group participants were asked to maintain normal activity levels and visited the physiotherapist once monthly. Five people in the intervention group did not complete the intervention, and one person from the control group dropped out of the study. Their data were not used for analyses. Of those who completed the intervention, two completed all 24 sessions, and 10 completed at least 20 sessions; no one completed more than half of the home exercise sessions. Significant differences were observed in the change scores between groups at 3 months for all outcomes except for the MSIS-29. Differences remained significant at 6 months for FAMS and MFIS only. The authors comment that the different results found in the two quality of life measures may be due to either being underpowered for the MSIS-29 or the questionnaires may have been sensitive to different dimensions of MS, where one (FAMS) is heavily weighted towards the psychosocial consequences of MS compared to the other measure. The small sample size and the clinical characteristics of the sample (i.e., independently mobile) may restrict the generalizability of the findings. Moreover, the method used to allocate the participants in the exercise or control groups may not have been truly random. (The researchers blindly pulled one of two pieces of paper labeled exercise or control to assign the individual during the consenting process, however, once the exercise group had 17 allocations, they assigned the rest of the eligible individuals to the control group.)
In 2008, Mutluay, Tekeoglu, Saip, Altintas, and Siva conducted a quasi-experimental study in Istanbul, Turkey, comparing two groups on the effectiveness of a group exercise intervention on motor impairments and the quality of life. Ninety outpatient clinic participants were first identified through clinical records and screened; 49 individuals with definite MS were found to be eligible. Individuals in a period of relapse, who had relapsed in the last 3 months, or whose EDSS score increased by a half point in the last 6 months were excluded, as were those with cognitive impairment and history of cardiovascular, respiratory, or orthopedic conditions. Twenty-eight participants were divided into four-person exercising groups based on their gender, disability levels, and clinical characteristics. Twenty-one participants who did not agree to partake in the exercise program constituted the control group. Neurological status, functional disability (Barthel index), fatigue (Fatigue Severity Scale), perceived exertion (Borg scale), muscle strength, mobility, and health-related quality of life (MSQOL-54) were measured for each participant. Data were collected from all participants at baseline and post intervention. No participants were lost to follow-up. The group exercise intervention consisted of six 2-hour weekly sessions. A trainer-physiotherapist supervised all sessions. Before and after each session, participants engaged in 30-minute casual social meetings where refreshments were provided. Six participants were unable to complete the exercise classes, and their data were excluded from analyses. Statistically significant improvements were seen in functional disability and other physical measures. The physical health (PHC) scores of the MSQOL-54 improved for those in the intervention group. The MHC scores did not show a significant improvement. The authors comment that perhaps the casual socialization period before and after the group exercise could be replaced with structured group psychotherapy sessions. No significant differences between the subgroups were found in any of the outcome measures. Since the subgroups were significantly different based on their EDSS scores, the authors conclude that this suggests that exercise was equally effective for people at different disability levels. One of the limitations of this study is that authors did not conduct intent-to-treat analyses. The authors also mention the lack of psychological assessment as another limitation; the MSQOL-54 (MHC) was the only measure used to assess how the intervention impacted this dimension. The fact that subjects were not randomly assigned to groups limits the validity of the findings.
Results from Prospective Cohort Studies
Stuifbergen, Blozis, Harrison, and Becker (2006) performed a longitudinal study of exercise, functional limitations, and quality of life among individuals with MS. Recruitment occurred through the National Multiple Sclerosis Society in the southwestern region of the United States and through advertisements in rural newspapers. The authors mailed recruitment information to n = 749 participants who remained eligible from the former study and enrolled a total of n = 611 study participants. At the end of the fifth year of data collection, 560 (90%) of the original participants remained. Study dropouts had greater functional limitations and were significantly older than those who remained in the 5-year study. The authors obtained self-reported measures of functional limitations and exercise including: the Incapacity Status Scale, a measure of functional limitations; the Health Promoting Lifestyle Profile II to assess engagement in activities to promote health and well-being (including exercise and physical activity); and the Quality of Life Index, MS version. Using latent curve modeling, the authors analyzed self-reported measures of functional limitations, quality of life, and exercise over time. The authors found that functional limitations scores were related to age and years since first diagnosis and were negatively correlated with exercise. An increase in functional limitations led to a decrease in quality of life and exercise. At baseline, after adjusting for background variables, exercise was associated with lower functional limitations and more positive quality of life. Exercise at baseline was not associated with age and gender. Those who exercised more at the beginning of the study reported less accumulation of functional limitations over the 5-year study period. The authors concluded that individuals with MS might slow the trajectory of increasing functional limitations over time with consistent exercise. Limitations of this study include use of self-report measures of exercise and limitations.
In order to understand the explanatory role of worsening MS symptoms in reducing physical activity, Motl and colleagues (2008) conducted a prospective cohort study examining worsening of symptoms and self-reported physical activity over a 3-to-5-year period. The study involved 51 participants with MS, with different courses of disease. In addition to course of MS, a neurologist assessed EDSS score and depression score as measured by Chicago Multiscale Depression Inventory, and these were included in analysis as covariates. Worsening of symptoms was assessed by the question “Since you were last tested for this project, have you experienced any worsening of your MS symptoms?” The International Physical Activity Questionnaire (IPAQ) served as the self-report measure for physical activity. The primary finding was that worsening of symptoms across a 3-to-5-year period was associated with lower levels of self-reported physical activity independent of depression, neurological disability, and MS disease course. The authors recommend that management of symptoms may have an important role to play in exercise adherence and promotion of exercise as a method to manage symptoms. More research is needed to test the direction of relationship between symptoms and exercise, and the authors recommend using measures of worsening symptoms with continuous—as opposed to dichotomous—scales.
Motl and McAuley (2009) conducted a prospective cohort study to examine the hypothesized associations of depression, fatigue, pain, social support, self-efficacy, and symptoms with changes in physical activity and quality of life. Participants wore an accelerometer for 7 days and were subsequently assessed at baseline (n = 292) and 6 months (n = 276) using a number of questionnaires. Questionnaires were related to measures of physical activity, quality of life, disability, fatigue, symptoms of depression, pain, self-efficacy, and social support. Symptoms of depression were measured using the Hospital Anxiety and Depression Scale. Quality of life was assessed using the Leeds Quality of Life Multiple Sclerosis Scale and the Satisfaction with Life Scale. Perceived fatigue was measured using the Fatigue Severity Scale. Self-efficacy was measured using the Multiple Sclerosis Self-Efficacy Scale. Pain was measured using the short-form McGill Pain Questionnaire. Social support was measured using the Social Provisions Scale. Physical activity was measured using the Godin Leisure Time Activity Scale. Results confirmed the hypotheses that increased physical activity is indirectly associated with increased quality of life, with intermediary pathways of fatigue, pain, social support, and self-efficacy. Contrary to the authors’ hypotheses, change in depression was not associated with an increase of physical activity. This lack of association between physical activity and depression may have been affected by the relatively low levels of depression among participants in this sample at baseline, creating a floor effect. Other limitations of this study and its findings include a relatively short intervention and follow-up period. There may be limited generalizability due to a predominantly white, female sample although the majority of individuals diagnosed with MS are of this demographic description.
Results from Cross-Sectional Studies
In the context of findings of other studies showing an indirect relationship between physical activity and quality of life in persons with MS, Motl, McAuley, Snook, and Gliottoni (2009) conducted a study to examine the relationship between physical activity and QOL of persons with MS. The research group recruited a convenience sample of individuals who were members of the local chapters of the MS society, with a definite diagnosis of MS, who were relapse free in the last 30 days, and who were ambulatory with minimal assistance. Individuals were recruited through research announcements mailed to past study participants, advertisements in MS society publications, and email messages to members. The final sample consisted of 292 individuals, with 245 females and 47 males. Data were collected through self-administered questionnaires on physical activity (Godin Leisure Time Exercise Questionnaire), quality of life (Leeds Quality of Life Multiple Sclerosis Scale), disability (Patient-Determined Disease Steps), fatigue (Fatigue Severity Scale), mood (Hospital Anxiety and Depression Scale), pain (McGill Pain Questionnaire), self-efficacy (Multiple Sclerosis Self-Efficacy Scale), and social support (Social Provisions Scale). Participants were asked to wear an accelerometer for a 7-day period and to complete the questionnaires on the 8th day. The authors tested two models: one examining the direct association between physical activity and QOL and another examining the indirect association between these two variables, with the intermediate variables included in the model. As hypothesized, they found statistically significant positive correlation between physical activity and quality of life. Moreover, they found that this sample of individuals with MS who were more physically active reported lower levels of depression, fatigue and pain, and higher levels of social support and self-efficacy for managing MS. These factors were also associated with better quality of life, further supporting the indirect relationship between physical activity and quality of life of persons with MS. Because this is a cross-sectional, correlational study, causation among variables cannot be determined. The findings are limited in their generalizability due to the use of a convenience sample that may have attracted people who were already more physically active than the average individual with MS, and also due to demographic characteristics of the sample, which was primarily Caucasian women.
Stroud and Minahan (2009) conducted a cross-sectional study of fatigue, depression, and quality of life scores based on exercise level among persons with various levels of MS. They sent out survey questionnaires with measures of activity levels and outcome variables. Four hundred and eighteen individuals from Australian databases of MS patients were invited to participate and were sent questionnaires. Of the invited individuals, 130 returned questionnaires: 9 of these were excluded either because they were incomplete or because the reported activity level was not representative of the subject’s usual activity level. Participants included 121 individuals with MS, mild-moderate as well as more severe MS. Based on the responses to the survey items about physical activity level, participants were classified as exercisers (n = 52, those who exercised at least 30 minutes twice weekly) and non-exercisers (n = 69). The outcomes on other variables were then correlated with exercise. MS diagnoses were confirmed by a neurologist or other physician, with disease course and severity reported by participants. Participants were measured on the dimensions of fatigue, depression, physical activity, and quality of life. Measures included the Beck Depression Inventory (21 items), Modified Fatigue Impact Scale, International Physical Activity Questionnaire, Multiple Sclerosis Impact Scale (29 items, measures disease severity), Disease Step Scale (measures disability status), and the Health Status Questionnaire Short Form (36 items), which was used to measure quality of life and produces mental health and physical health composite scores. The group that reported exercising at least 30 minutes twice weekly experienced better scores with regard to depression, fatigue, and quality of life. Interaction effects were found for exercise status and disease severity with regard to quality of life scores. These results suggested that individuals with moderate MS in particular might improve more in quality of life with exercise. Limitations included patient report of MS diagnosis. Additionally, due to the cross-sectional nature of the study, causality could not be assessed. Another limitation was that participants were recruited from two separate databases and analyses were not conducted to assess whether there were significant differences in these populations at baseline. The relatively low response rate of 31% suggests the possibility that data were limited by potential selection effects of more athletic individuals participating in the study and thus being over-represented in the sample. Lastly, due to the de-identification of the data as they were collected, differences in responders and nonresponders to the study were not assessed.
Turner, Kivlahan, and Haselkorn (2009) conducted a cross-sectional study examining a sample of U.S. military veterans with MS and the association of exercise with quality of life, including physical and mental health. They also examined “participation,” which was conceptualized—as in the International Classification of Functioning, Disability and Health—as the “lack of involvement in community, social, occupational, and other meaningful and desirable life pursuits.” Little is known about the relationship between participation restriction and exercise. The authors analyzed self-administered survey data collected in 1999 from n = 2,995 veterans who received services in the Veterans Health Administration from 1998 to 2004 and whose MS diagnosis was verified through treatment or hospitalization. Questionnaire data were collected on medical comorbidity (Seattle Index of Comorbidity), physical functioning, and mental health (VR-36, the VA version of the SF-36), and participation restriction (Role Physical, Role Emotional, and Social Functioning scales of the VR-36), and bodily pain (VR-36). Multiple logistic regression results showed that exercise among people with MS was less common with increasing age and higher levels of bodily pain. Education, living situation (i.e., living alone), and higher body mass index (BMI) were associated with higher likelihood of exercise in this study population. After adjusting for demographic variables and medical comorbidities, exercise was also associated with better physical functioning; a modest association was also found between exercise and mental functioning. After controlling for demographics, medical comorbidities, and both physical and mental health status, presence of exercise was also associated with better social and role functioning, thus leading to greater participation. Sample characteristics were older, and disproportionately non-Caucasian. Results may also not generalize to people with MS who are not veterans. Due to the cross-sectional design of the study, no causal relationships among exercise and quality of live variables can be determined.
Motl and colleagues (2010) performed a cross-sectional survey of individuals with relapsing-remitting MS in an attempt to better understand the relationships among factors related to physical activity. The rationale for the study was that general symptoms in MS are perceived as a correlate of reduced activity, but that little is known about specific symptoms as correlates. The authors recruited participants for this study through national and state MS societies and screened 463 individuals. The final sample meeting the inclusion criteria and willing to participate was n = 269. The authors examined several physical dimensions of MS functioning, including the MS Related Symptom Checklist, the Fatigue Severity Scale, the Hospital Anxiety and Depression Scale, the McGill Pain Questionnaire, and the Grodin Leisure Time Exercise Questionnaire. Participants were asked to wear an accelerometer for 1 week. Several rounds of structural equation modeling analyses were then conducted and the following results found: Fatigue and depression, but not symptoms, had a statistically significant, direct association with physical activity. Neurological impairment had a statistically significant direct association with symptoms, fatigue, and physical activity—but not depression. The association between physical activity and symptoms was indirect and accounted for by fatigue and depression. The authors conclude that these results provide evidence that two symptoms, fatigue and depression, are independent and proximal correlates of physical activity in individuals with relapsing-remitting MS.
Suh, Motl, and Mohr in 2010 sought to address the gaps in knowledge about correlates of psychological well-being in early MS. They conducted a correlational study with 96 participants. The purpose of the study was to examine the association between physical activity and psychological well-being in early MS. Physical activity was measured using an accelerometer that the participants wore for 7 days. The data were used to calculate an estimate of weekly physical activity. Participants then completed the Patient-Determined Disease Steps to determine disability and Hospital Anxiety and Depression Scale to determine psychological well-being. No significant associations were found between physical activity and anxiety or disability and anxiety, a path model was not tested for anxiety. Although the direct association between physical activity and depression was not significant, the indirect association was found to be significant. The associations between physical activity and disability, and between disability and depression were significant whether the path model was one with direct or indirect effect between physical activity and depression. The associations remained significant even with the introduction of effects of gender, age, employment, education, income, and MS duration on physical activity, disability, and depression. These results point to the importance of physical activity as a behavioral method of reducing disability and thereby improving well-being in the early stages of MS. However, the authors acknowledge that the direction of causality is not clear from this study design, and that it is alternatively likely that disability might influence depression through effects on physical activity. Further the sample of largely white, well-educated women with annual income exceeding $40,000 limits generalizability.
Return to top
Conclusions from Experimental Studies
Taken together, results of experimental studies provide some evidence that certain types of exercise (aerobic rather than resistance training, and perhaps yoga) can affect quality of life and various dimensions of mood. The key findings are as follows:
- Participation in an exercise intervention can improve various psychosocial dimensions of self-reported quality of life and/or mood for individuals with mild to moderate MS (Bombardier et al., 2011; Dalgas et al., 2010; McCullagh, Fitzgerald, Murphy, & Cooke, 2008; Mostert & Kesselring, 2002; Petajan et al., 1996; Solari et al., 1999; Sutherland et al., 2001). No body of evidence exists demonstrating the psychological effects of exercise on people with more severe MS.
- There is no body of evidence at present that indicates exercise interventions can affect cognitive functioning (Oken et al., 2004; Velikonja et al., 2010).
- Changes in quality of life and depression are most apt to be effected through various types of aerobic training, e. g., arm and leg aerobics (Petajan et al., 1996); water aerobics (Sutherland et al., 2001); bicycle aerobics (Mostert & Kesselring, 2002); exercise classes with variety of exercises emphasizing aerobics (McCullagh et al., 2008) and physical activity and exercise counseling which could include aerobic exercises (Bombardier et al., 2011). There is no strong evidence that a particular exercise intervention can outperform any other.
- Studies of endurance training (Dettmers et al., 2009) and progressive resistance training (Dalgas et al., 2010) have not generated consistent effects on mood and quality of life (Sabapathy et al., 2010).
- Studies of yoga are few and contradictory, demonstrating an effect (Ahmadi et al., 2010) or no effect (Oken et al., 2004; Velikonja et al., 2010) on mood, quality of life, and psychosocial measures.
- The reason exercise interventions impact quality of life dimensions and mood are unknown and may be partially due to the exercise intervention typically occurring in a group setting with social support (McAuley et al., 2007; Romberg et al., 2005; Sutherland et al., 2001).
Conclusions from Non-Experimental Studies
Taken together, results of non-experimental studies suggest that exercise and physical activity are positively associated with quality of life and various aspects of mood. The key findings are as follows:
- Consistent with the results of experimental studies, there is evidence that exercise is associated with lower depression scores and more positive quality of life scores (Rasova et al., 2006; Stroud & Minahan, 2009; Stuifbergen et al., 2006; Turner et al., 2009). Trait anxiety may be a moderator of mood improvements associated with exercise in MS (Petruzello, Snook, Gliottoni, & Motl, 2009)
- Increased physical activity is associated with higher quality of life, less depression, fatigue and pain, and better self-esteem among individuals with MS (Motl & McAuley, 2009; Motl, McAuley, Snook, & Gliottoni, 2009; Motl et al., 2010; Suh et al., 2010).
- Fatigue and depression rather than overall symptoms or pain may affect levels of physical activity in persons with MS. Relationships among these factors are complex and need more study (Motl et al., 2009; Motl & McAuley, 2009; Motl et al., 2010; Suh et al., 2010).
- Worsening of MS symptoms is associated with lower levels of physical activity. (Motl et al., 2008) and the presence of anxiety may negatively affect mood improvements associated with exercise in MS (Petruzello et al., 2009).
Acknowledgements and Statement Concerning Conflict of Interest
None of the authors report a conflict of interest. The authors would like to thank the National Institute on Rehabilitation Research for their support of this grant and the National MS Society, particularly Dr. Nick LaRocca, for support of this systematic review.
Return to top
Appendix A: Table of All Studies Reviewed
| Authors | Published | Research Design | Intervention | N | Dependent Variables | Outcomes / Major Findings |
| Petajan, J. H., et al. | 1996 | RCT | 15 weeks aerobic training | Experimental n = 21 Control n = 25 | Daily activities, mood, fatigue, and disability status | No significant improvements were noted in depression, anger, and psychosocial factors over time. |
| Solari, A., et al. | 1999 | RCT | 3-week inpatient physical rehabilitation involving twice daily structured exercise program | Experimental n = 27
Control n = 23 |
Disability, health status, QOL | Experimental group had significant improvement only on mental health index of SF-36. |
| Sutherland, G., Andersen, M. B., & Stoove, M. A. | 2001 | RCT | 10-week aerobic exercise | Experimental n = 11
Control n = 11 |
HRQOL and psychological well-being | Exercise had positive effect on well-being and mood, including improvements in pain, tension, social and sexual functioning, vigor/fatigue, and energy. |
| Mostert, S., & Kesselring, J. | 2002 | RCT: four-group design | 4-week bicycle-based exercise training | Experimental n = 13
Control n = 13 |
Health perception, social interaction, activity level | Significant improvement found in aerobic threshold, vitality and social functioning indexes of SF-36 in experimental group. |
| Oken, B. S., et al. | 2004 | RCT | 26 weeks yoga, 26 weeks aerobic exercise, compared with wait-list controls | Yoga n = 26
Exercise n = 21 Wait-List control n = 22 |
Cognitive function, fatigue, mood, and QOL | Exercise groups scored better on SF-36 vitality measure and multidimensional fatigue measure, but there was no significant impact on depression. |
| Schulz, K.-H., et al. | 2004 | RCT: wait-list controlled trial | 8-week aerobic bicycle training | Study 1: immune-endocrine study,
n = 28; exercise n = 15; control n = 13. Study 2: coordinative extension study, n = 39; exercise n = 23; control n = 16. |
QOL, affect, fatigue, coordinative function, and psychological function. + inflammatory cytokine activity | Significant improvement noted in disease-specific quality of life. |
| Romberg, A., Virtanen, A., & Ruutiainen, J. | 2005 | RCT | 6-month progressive exercise | Experimental n = 47
Control n = 48 |
Functional impairment and HRQOL | Leg function and movement improved in exercise group. No differences were noted in QOL dimensions. |
| McAuley, E., Motl, R.W., Morris, K.S., et al. | 2007 | RCT | Self-efficacy enhancement intervention | Experimental n = 13
Control n = 13 |
Physical activity, well-being, and affective response | Intervention group had moderate improvement in exercise adherence, improved affective response after exercise, and stable level of satisfaction with life through 3-month follow-up. |
| Dettmers, C., Sulzmann, M., Ruchay-Plossl, A., Gutler, R., & Vieten, M. | 2009 | RCT | 3-week endurance training compared with 3-week intervention including stretching, balancing, and coordination |
Experimental n = 15
Control n = 15 |
Walking, fatigue, depression, and QOL | Significant differences in walking distance and walking time in endurance training group. No differences between groups or within-group changes in other dimensions. |
| Ahmadi, A., Nikbakh, M., Arastoo, A. A., & Habibi, A.-H. | 2010 | RCT | 8 weeks of Hatha Yoga | Experimental n = 11
Control n = 10 |
Balance, speed, endurance of walking, fatigue, and QOL | Yoga group had better walking speed, endurance, lower fatigue levels and greater improvements in physical function, emotional well-being, and cognitive function, as well as physical and mental health composite scores. |
| Dalgas et al. | 2010 | RCT | 12-week progressive resistance training | Control n = 15
Exercise n = 16 |
Fatigue, depression, QOL | Results indicated improvements in fatigue, depression scores, and quality of life for the exercise group, which were maintained at the 12-week follow-up. |
| Sabapathy, N.M., Minahan, C.L., Turner, G.T., & Broadley, S. A. | 2010 | RCT: Cross-over design | 8 weeks each of endurance training and resistance-exercise training with 8-week wash-out period | N = 16 | Physical ability, disease impact, fatigue, depression, and QOL | No differences noted in outcomes between the two training programs; both resulted in improved physical ability. Improvements were noted on psychosocial scale of MFIS alone after 8 weeks of exercise training. |
| Velikonja, O., Curic, K., Ozura, A., & Jazbec, S. S. | 2010 | RCT | 10 weeks of sports climbing and 10 weeks of yoga | N = 20 | Cognitive function, mood, and fatigue | Significant reduction of EDSS pyramidal functions score in the SC group. Subjects in yoga group had significant improvement in selective attention only. SC group alone had a significant reduction in level of fatigue, with reduced impact of fatigue on physical and cognitive function, but not on psychosocial function. |
| Bombardier et al. | 2011 | RCT | Telephone counseling to increase physical activity over a 12-week period | Experimental n = 44
Control n = 48 |
Symptoms of depression | No significant difference noted between groups on primary outcome (that is, at least 50% reduction in HAM-D score). Secondary outcome analysis by examination of effects using the HAM-D as a continuous measure showed that the intervention group reported significantly lower post-treatment depression severity compared to controls. Intervention group also reported significantly greater physical activity at 12 weeks. |
| Rasova, K., et al. | 2006 | Quasi-experimental | Neurophysio-logically based physiotherapy only, aerobic training only, combination of the two, or no intervention control | Group #1: n=24, Group #2: n=36, Group #3: n=19, and Group #4: n=16 | Impairment, disability, handicap, QOL, fatigue, depression, respiratory function, and physical fitness | Imbalanced groups did not permit between-groups analysis. Within-group analysis showed significant improvement in depression in all groups that received an intervention. |
| McCullagh, R., Fitzgerald, A.P., Murphy, R.P., & Cooke, G. | 2008 | Quasi-experimental | 12-week exercise program | Experimental n = 17
Control n = 13 |
Fatigue, QOL | Significant differences were observed at 6-month follow-up in fatigue and in QOL as measured by FAMS only, not MSIS-29. |
| Mutluay, F. K., Tekeoglu, A., Saip, S., Altintas, A., & Siva, A. | 2008 | Quasi-experimental | 6-week group exercise program | Experimental n = 28 Control n = 21 | Disability and QOL | Significant improvements were seen in functional disability level, perceived exertion, muscle strength, and mobility in the intervention group. |
| Stuifbergen, A. K., Blozis, S. A., Harrison, T. C., & Becker, H. A. | 2006 | Prospective cohort | No intervention | N = 611 | Trajectories and interactions of functional limitations, health (exercise) behaviors, and QOL | Functional limitations scores were related to age and years since first diagnosis and were negatively correlated with exercise. Ongoing participation in exercise was significantly related to decreased rates of change in functional limitations. |
| Motl, R.W., et al. | 2008 | Prospective cohort | No intervention | N = 51 | Relationship between symptoms and physical activity over time | Worsening of symptoms across a 3-to-5-year period was associated with lower levels of self-reported physical activity independent of depression, neurological disability, and MS disease course. |
| Motl, R.W. & McAuley, E. | 2009 | Prospective cohort | No intervention | Baseline n = 292
6-month follow-up n = 276 |
Associations between physical activity; and fatigue, pain, social support, self-efficacy; and QOL | Increased physical activity was indirectly associated with improved QOL, with intermediary pathways of fatigue, pain, social support, and self-efficacy. |
| Motl, R.W., McAuley, E., Snook, E.M., & Gliottoni, R. C. | 2009 | Cross-sectional | No intervention | N = 292 | Associations between physical activity and QOL; and disability level, depression, fatigue, pain, social support, self-efficacy | Physical activity is significantly associated with QOL. The findings indicate disability, depression, pain, social support, and self-efficacy moderate the association. |
| Stroud, N.M., & Minahan, C.L. | 2009 | Cross-sectional | No intervention. Groups of exercisers and non-exercisers. | N = 121 | Fatigue, depression, QOL | Exercise group improved with regard to scores on depression, fatigue, and quality of life scales. Individuals with moderate MS in particular may improve more in quality of life with exercise. |
| Turner, A.P., Kivlahan, D.R., & Haselkorn, J.K. | 2009 | Cross-sectional | No intervention | N = 2995 | Exercise prevalence and associations with quality of life, including physical health, mental health, and participation restriction. | Exercise is associated with better physical, social, and role functioning. |
| Motl, R.W., et al | 2010 | Cross-sectional | No intervention | N = 269 | Physical activity association with fatigue, depression, pain | The association between physical activity and symptoms was indirect and accounted for by fatigue and depression. |
| Suh, Y., Motl, R.W., & Mohr, D.C. | 2010 | Cross-sectional | No intervention | N = 96 | Relationship between physical activity and psychological distress- anxiety and depression | The association between physical activity and depression in early MS is indirect by way of disability. |
Appendix B: Rating Scale for Rigor
Download – Rating Scale for Rigor
Appendix C: Rating Scale for Meaning and Perceived Utility
Download – Rating Scale for Meaning and Perceived Utility
Appendix D: References
+ Articles included in narrative synthesis
† Articles used only as background information for the narrative synthesis
* Articles excluded from the narrative synthesis after rating for quality due to low methodology scores
° Instruments used for rating articles
+ Ahmadi, A., Nikbakh, M., Arastoo, A. A., Habibi, A.-H. (2010). The effects of a yoga intervention on balance, speed and endurance of walkingm fatigue and quality of life in people with multipe sclerosis. Journal of Human Kinetics, 23, 71–78.
Armstrong, L. E., Winant, D. M., Swasey, P. R., Seidle, M. E., Carter, A. L., & Gehlsen, G. (1983). Using isokinetic dynamometry to test ambulatory patients with multiple sclerosis. Physical Therapy, 63(8), 1274–1279.
Asano, M., Dawes, D. J., Arahaf, A., Moriello, C., & Mayo, N. E. (2009). What does a structured review of the effectiveness of exercise interventions for persons with multiple sclerosis tell us about the challenges of designing trials? Multiple Sclerosis, 15, 412–421.
Bakshi, R., Shaikh, Z. A., Miletich, R. S., Czarnecki, D., Dmochowski, J., Henschel, K.,…Kinkel, P. R. (2000). Fatigue in multiple sclerosis and its relationship to depression and neurologic disability. Multiple Sclerosis, 6, 181–185.
Barrett, C. L., Mann, G. E., Taylor, P. N., & Strike, P. ( 2009). A randomized trial to investigate the effects of functional electrical stimulation and therapeutic exercise on walking performance for people with multiple sclerosis. Multiple Sclerosis, 15, 493–504.
* Bjarnadottir, O. H., Konradsdottir, A. D., Reynisdottir, K., & Olafsson, E. (2007). Multiple sclerosis and brief moderate exercise. A randomised study. Multiple Sclerosis, 13, 776–782.
+ Bombardier, C. H., Ehde, D. M., Gibbons, L. E., Wadhwani, R., & Sullivan, M. (2011). The efficacy of telephone-based physical activity promotion for major depression in people with multiple sclerosis: A randomized controlled trial. Pre-publication.
† Brown, T. R., & Kraft, G. H. (2005). Exercise and Rehabilitation for Individuals with Multiple Sclerosis. Physical Medicine and Rehabilitation Clinics of North America, 16, 213–255.
* Cakit, B. D., Nacir, B., Genc, H., Saracoglu, M., Karagoz, A., Erdem, H. R., & Ergun, U. (2010). Cycling Progressive Resistance Training for People with Multiple Sclerosis: A Randomized Controlled Study. American Journal of Physical Medicine and Rehabilitation, 89(6), 446–457.
Cartlidge, N. E. F. (1972). Autonomic function in multiple sclerosis. Brain, 95, 661–664.
Chen, W.-Y., Pierson, F. M., & Burnett, C. N. (1987). Force-time measurements of knee muscle functions of subjects with multiple sclerosis. Physical Therapy, 67(6), 934–940.
Chiara, T., Carlos, J., Martin, D., Miller, R., & Nadeau, S. (1998). Cold effect on oxygen uptake, perceived exertion, and spasticity in patients with multiple sclerosis. Archives of Physical Medicine and Rehabilitation, 79, 523–528.
+ Dalgas, U., Stenager, E., Jakobsen, J., Petersen, T., Hansen, H. J., Knudsen, C.,…Ingemann-Hansen, T. (2010). Fatigue, mood and quality of life improve in MS patients after progressive resistance training. Multiple Sclerosis, 16(4), 480–490.
de Haan, A., de Ruiter, C. J., van der Woude, L. H. V., & Jongen, P. J. H. (2000). Contractile properties and fatigue of quadriceps muscles in multiple sclerosis. Muscle Nerve, 23, 1534–1541.
de Ruiter, C. J., Jongen, P. J. H., van der Woude, L. H. V., & de Haan, A. (2001). Contractile speed and fatigue of adductor pollicis muscle in multiple sclerosis. Muscle Nerve, 24, 1173–1180.
DeBolt, L. S., & McCubbin, J. A. (2004). The effects of home-based resistance exercise on balance, power, and mobility in adults with multiple sclerosis. Archives of Physical Medicine and Rehabilitation, 85, 290–297.
Desharnais, R., Jobin, J., Cote, C., Levesque, L., & Godin, G. (1993). Aerobic exercise and the placebo effect. Psychosomatic Medicine, 55, 149–154.
+ Dettmers, C., Sulzmann, M., Ruchay-Plossl, A., Gutler, R., & Vieten, M. (2009). Endurance exercise improves walking distance in MS patients with fatigue. Acta Neurologica Scandinavica, 120, 251–257.
DiFabio, R. P., Soderberg, J., Choi, T., Hansen, C. R., & Schapiro, R. T. (1998). Extended outpatient rehabilitation: Its influence on symptom frequency, fatigue, and functional status for persons with progressive multiple sclerosis. Archives of Physical Medicine and Rehabilitation, 79, 141–146.
Dodd, K. J., Taylor, N. F., Denisenko, S., & Prasad, D. (2006). A qualitative analysis of a progressive resistance exercise programme for people with multiple sclerosis. Disability and Rehabilitation, 28(18), 1127–1134.
† Farkas, M., Rogers, E. & Anthony, W., (2008). Systematic review procedures for rating the rigor and the meaning of disability research. Boston: Boston University, Center for Psychiatric Rehabilitation.
° Farkas, M., & Anthony, W., (2008). Standards for Rating the Meaning of Disability Research. Boston: Boston University, Center for Psychiatric Rehabilitation.
† Ferrans, C. E., & Powers, M. J. (1985). Quality of life index: development and psychometric properties. Advances in Nursing Science, 8(1), 15–24.
Filippi, M., & Rocca, M. A. (2003). Disturbed function and plasticity in multiple sclerosis as gleaned from functional magnetic resonance imaging. Current Opinion in Neurology, 16, 275–282.
* Finkelstein, J., Lapshin, O., Castro, H., Cha, E., & Provance, P. G. (2008). Home-based physical telerehabilitation in patients with multiple sclerosis: A pilot study. Journal of Rehabilitation Research and Development, 45(9), 1361–1374.
Foglio, K., Clini,E., Facchetti, D., Vitacca, M., Marangoni, S., Bonomelli, M., & Ambrosino, N. (1994). Respiratory muscle function and exercise capacity in multiple sclerosis. European Respiratory Journal, 7, 23–28.
Fragoso, Y. D., Santana, D. L. B., & Pinto, R. C. (2008). The positive effects of a physical activity program for multiple sclerosis patients with fatigue. Neuro Rehabilitation, 23, 153–157.
* Freeman, J., & Allison, R. (2004). Group exercise classes in people with multiple sclerosis: a pilot study. Physiotherapy Research International, 9(2), 104–107.
† Gallien, P., Nicolas, B., Robineau, S., Petrilli, S., Houedakor, J., & Durufle, A. (2007). Physical training and multiple sclerosis. Annales de réadaptation et de médecine physique, 50, 373–376.
* Giesser, B., Beres-Jones, J., Budovitch, A., Herlihy, E., & Harkema, S. (2007). Locomotor training using body weight support on a treadmill improves mobility in persons with multiple sclerosis: a pilot study. Multiple Sclerosis, 13, 224–231.
Gold, S. M., Schulz, K.-H., Hartmann, S., Mladek, M., Lang, U. E., Hellweg, R.,…Heesen, C. (2003). Basal serum levels and reactivity of nerve growth factor and brain-derived neurotrophic factor to standardized acute exercise in multiple sclerosis and controls. Journal of Neuroimmunology, 138, 99–105.
Gosselink, R., Kovacs, L., & Decramer, M. (1999). Respiratory muscle involvement in multiple sclerosis. European Respiratory Journal, 13, 449–454.
Gosselink, R., Kovacs, L., Ketelaer, P., Carton, H., & Decramer, M. (2000). Respiratory muscle weakness and respiratory muscle training in severely disabled multiple sclerosis patients. Archives of Physical Medicine and Rehabilitation, 81, 747–751.
† Hart, S., Fonareva, I., Merluzzi, N., & Mohr, D. C. (2005). Treatment for depression and its relationship to improvement in quality of life and psychological well-being in multiple sclerosis. Quality of Life Research, 14(3), 695–703.
Harvey, L., Smith, A. D., & Jones, R. (1999). The effect of weighted leg raises and quadriceps strength, EMG parameters and functional activities in people with multiple sclerosis. Physiotherapy, 85(3), 154–161.
† Heesen, C., Romberg, A., Gold, S., & Schulz, K.-H. (2006). Physical exercise in multiple sclerosis: supportive care or a putative disease-modifying treatment. (Report). Expert Review of Neurotherapeutics, 6(3), 347–349.
† Hobart, J., Lamping, D., Fitzpatrick, R., Riazi, A., & Thompson, A. (2001). The multiple sclerosis impact scale (MSIS-29): A new patient-based outcome measure. Brain, 124, 962–973.
Husted, C., Pham, L., Hekking, A., & Niederman, R. (1999). Improving quality of life for people with chronic conditions: the example of T’ai chi and multiple sclerosis. Alternative Therapies in Health and Medicine, 5(5), 70–74.
Iriarte, J., & de Castro, P. (1998). Correlation between symptom fatigue and muscular fatigue in multiple sclerosis. European Journal of Neurology, 5, 579–585.
Janssens, A. C. J. W., van Doorn, P. A., de Boer, J. B., Kalkers, N. F., van der Meche, F. G. A., Passchier, J., & Hintzen, R. Q. (2003). Anxiety and depression influence the relation between disability status and quality of life in multiple sclerosis. Multiple Sclerosis, 9, 397–403.
Joffe, R. T., Lippert, G. P., Gray, T. A., Sawa, G., & Horvath, Z. (1987). Mood disorder and multiple sclerosis. Archives of Neurology, 44, 376–378.
Johnson, K. B. (1996). Comment: Exercise, drug treatment, and the optimal care of multiple sclerosis patients. Annals of Neurology, 39(4), 422–423.
Johnson, S. K., Frederick, J., Kaufman, M., & Mountjoy, B. (1999). A controlled investigation of bodywork in multiple sclerosis. The Journal of Alternative and Complimentary Medicine, 5(3), 237–243.
Kasser, S. (2009). Exercising with multiple sclerosis: insights into meaning and motivation. Adapted Physical Activity Quarterly: APAQ, 26(3), 274–289.
Kent-Braun, J. A., Sharma, K. R., Miller, R. G., & Weiner, M. W. (1994). Post-exercise phosphocreatine resynthesis is slowed in multiple sclerosis. Muscle & Nerve, 17(8), 835–841.
Kent-Braun, J. A., Sharma, K. R., Weiner, M. W., & Miller, R. G. (1994). Effects of exercise on muscle activation and metabolism in multiple sclerosis. Muscle & Nerve, 17(10), 1162–1169.
* Koseoglu, B. F., Gokkaya, N. K. O., Ergun, U., Inan, L., & Yesiltepe, E. (2006). Cardiopulmonary and metabolic functions, aerobic capacity, fatigue and quality of life in patients with multiple sclerosis. Acta Neurologica Scandanavica, 114, 261–267.
† Kurtzke, J. F. (1983). Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology, 33, 1444–1452.
Lambert, C. P., Archer, R. L., & Evans, W. J. (2001). Muscle strength and fatigue during isokinetic exercise in individuals with multiple sclerosis. Medicine & Science in Sports & Exercise, 33(10), 1613–1619.
Latash, M., Kalugina, E., Nicholas, J., Orpett, C., Stefoski, D., & Davis, F. (1996). Myogenic and central neurogenic factors in fatigue in multiple sclerosis. Multiple Sclerosis, 1(4), 236–241.
Lublin, F., & Reingold, S. C. (1996). Defining the clinical course of multiple sclerosis: Results of an international survey. Neurology, 46(4), 907–911.
Malcomson, K. S., Dunwoody, L., & Lowe-Strong, A. S. (2007). Psychosocial interventions in people with multiple sclerosis: A review. Journal of Neurology, 254, 1–13.
+ McAuley, E., Motl, R. W., Morris, K. S., Hu, L., Doerksen, S. E., Elavsky, S., & Konopack, J. F. (2007). Enhancing physical activity adherence and well-being in multiple sclerosis: a randomised controlled trial. Multiple Sclerosis, 13, 652–659.
+ McCullagh, R., Fitzgerald, A. P., Murphy, R. P., & Cooke, G. (2008). Long-term benefits of exercising on quality of life and fatigue in multiple sclerosis patients with mild disability: a pilot study. Clinical Rehabilitation, 22, 206–214.
Mevellec, E., Lamotte, D., Cantalloube, S., Amarenco, G., & Thoumie, P. (2003). Relationship between gait speed and strength parameters in multiple sclerosis. Annales de réadaptation et de médecine physique, 46, 85–90.
* Mills, N., Allen, J., & Morgan, C. (1999). Does Tai Chi/Qi Gong help patients with multiple sclerosis. Journal of Bodywork and Movement Therapies, 4(1), 39–48.
† Moher, D., Schulz, K. F., & Altman, D. G. (2001). The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Lancet, 357(9263), 1191–1194.
Mohr, D. C., Boudewyn, A. C., Goodkin, D. E., Bostrom, A., & Epstein, L. (2001). Comparative outcomes for individual cognitive-behavior therapy, supportive–expressive group psychotherapy, and sertraline for the treatment of depression in multiple sclerosis. Journal of Consulting and Clinical Psychology, 69(6), 942–949.
Mohr. D. C., Burke, H., Beckner, V., & Merluzzi, N. (2005). A preliminary report on a skills-based telephone-administered peer support programme for patients with multiple sclerosis. Multiple Sclerosis, 11, 222–226.
Mohr, D. C., Goodkin, D. E., Bacchetti, P., Boudewyn, A. C., Huang, L., Marrietta, P.,…Dee, B. (2000). Psychological stress and the subsequent appearance of new brain MRI lesions in MS. Neurology, 55, 55–61.
Moller, A., Wiedermann, G., Rohde, U., Backmund, H., & Sonntag, A. (1994). Correlates of cognitive impairment and depressive mood disorder in multiple sclerosis. Acta Psychiatrica Scandinavica, 89, 117–121.
+ Mostert, S., & Kesselring, J. (2002). Effects of a short-term exercise training program on aerobic fitness, fatigue, health perception and activity level of subjects with multiple sclerosis. Multiple Sclerosis, 8(2), 161–168.
+ † Motl, R. W., Arnett, P. A., Smith, M. M., Barwick, F. H., Ahlstrom, B., & Stover, E. J. (2008). Worsening of symptoms is associated with lower physical activity levels in individuals with multiple sclerosis. Multiple Sclerosis, 14, 140–142.
Motl, R. W., Dlugonski, D., Wojcicki, T. R., McAuley, E., & Mohr, D. C. (2011). Internet intervention for increasing physical activity in persons with multiple sclerosis. Multiple Sclerosis Journal, 17(1), 116–128.
Motl, R. W., & Gosney, J. L. (2008). Effect of exercise training on quality of life in multiple sclerosis: a meta-analysis. Multiple Sclerosis, 14, 129–135.
+ Motl, R. W., & McAuley, E. (2009). Pathways between Physical Activity and Quality of Life in Adults with Multiple Sclerosis. Health Psychology, 28(6), 682–689.
† Motl, R. W., McAuley, E., Snook, E. M., & Gliottoni, R. C. (2008). Does the relationship between physical activity and quality of life differ based on generic versus disease-targeted instruments? Annals of Behavioral Medicine, 36, 93–99.
+ Motl, R. W., McAuley, E., Snook, E. M., & Gliottoni, R. C. (2009). Physical activity and quality of life in multiple sclerosis: Intermediary roles of disability, fatigue, mood, pain, self-efficacy and social support. Psychology, Health, and Medicine, 14(1), 111–124.
+ Motl, R. W., McAuley, E., Wynn, D., Suh, Y., Welkert, M., & Dlugonski, D. (2010). Symptoms and Physical Activity Among Adults With Relapsing-Remitting Multiple Sclerosis. The journal of nervous and mental disease, 198(3), 213–219.
+ Mutluay, F. K., Tekeoglu, A., Saip, S., Altintas, A., & Siva, A. (2008). Group exercise training approach to multiple sclerosis rehabilitation. Nobel Medicus, 4(3), 20–26
† National Multiple Sclerosis Society. (2011). Brochures on General Information about MS. Retrieved from http://www.nationalmssociety.org/multimedia-library/brochures/general-information/index.aspx
Neill, J., Belan, I., & Ried, K. (2006). Effectiveness of non-pharmacological interventions for fatigue in adults with multiple sclerosis, rheumatoid arthritis, or systemic lupus erythematosus: a systematic review. Journal of Advanced Nursing, 56(6), 617–635.
Ng, A. V., Dao, H. T., Miller, R. G., Gelinas, D. F., & Kent-Braun, J. A. (2000). Blunted pressor and intramuscular metabolic responses to voluntary isometric exercise in multiple sclerosis. Journal of Applied Physilogy, 88, 871–880.
Nielsen, J. F., & Norgaard, P. (2002). Increased post-exercise facilitation of motor evoked potentials in multiple sclerosis. Clinical Neurophysiology, 113, 1295–1300.
† Nortvedt, M. W., & Riise, T. (2003). The use of quality of life measures in multiple sclerosis research. Multiple Sclerosis, 9, 63–72.
+ Oken, B. S., Kishiyana, S., Zajdel, D., Bourdette, D., Carlsen, J., Haas, M.,…Mass, M. (2004). Randomized controlled trial of yoga and exercise in multiple sclerosis. Neurology, 62, 2058–2064.
Oken, B. S., Zajdel, D., Kishiyama, S., Flegal, K., Dehen, C., Haas, M.,¼Leyva, J. (2006). Randomized, controlled, six-month trial of yoga in healthy seniors: Effects on cognition and quality of life. Alternative Therapies in Health and Medicine, 12(1), 40–47.
Olgiati, R., Jacquet, J., & Di Prampero, P. E. (1986). Energy cost of walking and exertional dyspnea in multiple sclerosis. American Review of Respiratory Disease, 134(5), 1005–1010.
† Olsen, L. R., Jensen, D. V., Noerholm, V., Martiny, K., & Bech, P. (2003). The internal and external validity of the Major Depression Inventory in measuring severity of depressive states. Psychological Medicine, 33, 351–356.
† Patten, S. B., Beck, C. A., Williams, J. V. A., Barbui, C., & Metz, L. M. (2003). Major depression in multiple sclerosis: A population-based perspective. Neurology, 61, 1524–1527.
Patti, F., Ciancio, M. R., Cacopardo, M., Reggio, E., Fiorilla, T., Palermo, F., … Thompson, A. J. (2003). Effects of a short outpatient rehabilitation treatment on disability of multiple sclerosis patients: A randomised controlled trial. Journal of Neurology, 250, 861–866.
Pepin, E. B., Hicks, R. W., Spencer, M. K., Tran, Z. V., & Jackson, C. G. R . (1996). Pressor response to isometric exercise in patients with multiple sclerosis. Medicine and Science in Sports and Exercise, 28(6), 656–660.
+ Petajan, J. H., Gappmaier, E., White, A. T., Spencer, M. K., Mino, L., & Hicks, R. W. (1996). Impact of aerobic training on fitness and quality of life in multiple sclerosis. Annals of Neurology, 39, 432–441.
Petajan, J. H., & White, A. T. (1999). Recommendations for physical activity in patients with multiple sclerosis. Sports Medicine, 27(3), 179–191.
Petajan, J. H., & White, A. T. (2000). Motor-evoked potentials in response to fatiguing grip exercise in multiple sclerosis patients. Clinical Neurophysiology, 111, 2188–2195.
* Petruzello, S. J., Snook, E. M., Gliottoni, R. C., & Motl, R. W. (2009). Anxiety and mood changes associated with acute cycling in persons with multiple sclerosis. Anxiety, Stress, and Coping, 22(3), 297–307.
* Pilutti, L. A., Lelli, D. A., Paulseth, J. E., Crome, M., Jiang, S., Rathbone, M. P., & Hicks, A. L. (2011). Effects of 12 Weeks of Supported Treadmill Training on Functional Ability and Quality of Life in Progressive Multiple Sclerosis: A Pilot Study. Archives of Physical Medicine and Rehabilitation, 92, 31–36.
* Plow, M. A., Mathiowetz, V., & Resnik, L. (2008). Multiple Sclerosis: Impact of physical activity on psychosocial constructs. American Journal of Health Behavior, 32(6), 614–626.
* Ponichtera-Mulcare, J. A., Mathews, T., Barrett, P. J., & Gupta, S. (1997). Change in aerobic fitness of patients with multiple sclerosis during a 6-month training program. Sports Medicine, Training and Rehabilitation, 7, 265–272.
Prakash, R. S., Snook, E. M., Motl, R. W., & Kramer, A. F. (2010). Aerobic fitness is associated with gray matter volume and white matter integrity in multiple sclerosis. Brain Research, 1341, 41–51.
* Rampello, A., Franceschini, M., Piepoli, M., Antenucci, R., Lenti, G., Olivieri, D., & Chetta, A. (2007). Effect of aerobic training on walking capacity and maximal exercise tolerance in patients with multiple sclerosis: A randomized crossover controlled study. Physical Therapy, 87(5), 545–555.
Rao, S. M. (1995). Neuropsychology of multiple sclerosis. Current Opinion in Neurology, 8, 216–220.
+ Rasova, K., Havrdova, E., Brandejsky, P., Zalisova, M., Foubikova, B., & Martinkova, P. (2006). Comparison of the influence of diferent rehabilitation programmes on clinical, spirometric and spiroergometric parameters in patients with multiple sclerosis. Multiple Sclerosis, 12, 227–234.
* Ratchford, J. N., Shore, W., Hammond, E. R., Rose, G., Rifkin, R., Nie, P.,¼Kerr, D. A. (2010). A pilot study of functional electrical stimulation cycling in progressive multiple sclerosis. Neurorehabilitation, 27, 121–128.
Rice, C. L., Vollmer, T. L., & Bigland-Ritchie, B. (1992). Neuromuscular responses of patients with multiple sclerosis. Muscle & Nerve, 15, 1123–1132.
† Rietberg, M. B., Brooks, D., Uitdehaag, B. M. J., & Kwakkel, G. (2004). Exercise therapy for multiple sclerosis. Cochrane Database of Systematic Reviews, Issue 3. Art. No.: CD003980. DOI: 10.1002/14651858.CD003980.pub2
° Rogers, E., Farkas, M., Anthony, W. & Kash, M, (2008). Standards for Rating Program Evaluation, Policy, Survey, Pre-post, or Correlational Human Subjects Studies. Boston: Boston University, Center for Psychiatric Rehabilitation.
+ Romberg, A., Virtanen, A., & Ruutiainen, J. (2005). Long-term exercise improves functional impairment but not quality of life in multiple sclerosis. Journal of Neurology, 252, 839–845.
Romberg, A., Virtanen, A., Ruutiainen, J., Aunola, S., Karppi, S.-L., Vaara, M.,¼Seppanen, A. (2004). Effects of a 6-month exercise program on patients with multiple sclerosis: A randomized study. Neurology, 63(11), 2034–2038.
† Rudick, R. A., Miller, D., Clough, J. D., Gragg, L. A., & Farmer, R. G. (1992). Quality of life in multiple sclerosis: Comparison with inflammatory bowel disease and rheumatoid arthritis. Archives of Neurology, 49, 1237–1242.
+ Sabapathy, N. M., Minahan, C. L., Turner, G. T., & Broadley, S. A. (2010). Comparing endurance- and resistance-exercise training in people with multiple sclerosis: a randomized pilot study. Clinical Rehabilitation, dol:10.117710269215510375908
Schapiro, R. T., Petajan, J. H., Kosich, D., Molk, B., & Feeney, J. (1988). Role of cardiovascular fitness in multiple sclerosis: A pilot study. Journal of Neurorehabilitation, 2(2), 43–49.
Schmid, W., & Aldridge, D. (2004). Active music therapy in the treatment of multiple sclerosis patients: A matched control study. Journal of Music Therapy, 41(3), 225–240.
+ Schulz, K.-H., Gold, S. M., Witte, J., Bartsch, K., Lang, U. E., Hellweg, R.,¼Heesen, C. (2004). Impact of aerobic training on immune-endocrine parameters, neurotrophic factors, quality of life and coordinative function in multiple sclerosis. Journal of the Neurological Sciences, 225, 11–18
Schwid, S. R., Thornton, C. A., Pandya, S., Manzur, K. L., Sanjak, M., Petrie, M. D.,…Goodman, A. D. (1999). Quantitative assessment of motor fatigue and strength in MS. Neurology, 53(4), 743–750.
Schyns, F., Paul, L., Finlay, K., Ferguson, C., & Noble, E. (2009). Vibration therapy in multiple sclerosis: a pilot study exploring its effects on tone, muscle force, sensation and functional performance. Clinical Rehabilitation, 23, 771–781.
Senaratne, M. P., Carroll, D., Warren, K. G., & Kappagoda, T. (1984). Evidence for cardiovascular autonomic nerve dysfunction in multiple sclerosis. Journal of Neurology, Neurosurgery & Psychiatry, 47, 947–952.
Sharma, K. R., Kent–Braun, J., Mynhier, M. A., Weiner, M. W., & Miller, R. G. (1995). Evidence of an abnormal intramuscular component of fatigue in multiple sclerosis. Muscle & Nerve, 18, 1403–1411.
Sharrack, B., Hughes, R. A. C., Soudain, S., & Dunn, G. (1999). The psychometric properties of clinical rating scales used in multiple sclerosis. Brain, 122, 141–159.
Sheean, G. L., Murray, N. M. F., Rothwell, J. C., Miller, D. H., & Thompson, A. J. (1997). An electrophysiological study of the mechanism of fatigue in multiple sclerosis. Brain, 120, 299–315.
† Snook, E. M., & Motl, R. W. (2009). Effect of Exercise Training on Walking Mobility in Multiple Sclerosis: A Meta-Analysis. Neurorehabilitation and Neural Repair, 23(2), 108–116.
+ Solari, A., Filippini, G., Gasco, P., Colla, L., Salmaggi, A., La Mantia, L.,¼Mendozzi, L. (1999). Physical rehabilitation has a positive effect on disability in multiple sclerosis patients. Neurology, 52(1), 57–62.
Stack, E. (2006). Editorial: Physiotherapy—the ultimate placebo. Physiotherapy Research International, 11(3), 127–128.
Storr, L. K., Sorensen, P. S., & Ravnborg, M. (2006). The efficacy of multidisciplinary rehabilitation in stable multiple sclerosis patients. Multiple Sclerosis, 12, 235–242.
+ Stroud, N. M., & Minahan, C. L. (2009). The impact of regular physical activity on fatigue, depression and quality of life in persons with multiple sclerosis. Health and Quality of Life Outcomes, 7(68). doi:10.1186/1477-7525-7-68
Stuifbergen, A. K., & Becker, H. (2001). Health promotion practices in women with multiple sclerosis. Physical Medicine and Rehabilitation Clinics of North America, 12(1), 9–22.
+ Stuifbergen, A. K., Blozis, S. A., Harrison, T. C., & Becker, H. A. (2006). Exercise, functional limitations, and quality of life: A longitudinal study of persons with multiple sclerosis. Physical Medicine and Rehabilitation, 87, 935–943.
+ Suh, Y., Motl, R. W., & Mohr, D. C. (2010). Physical activity, disability, and mood in the early stage of multiple sclerosis. Disability and Health Journal, 3, 93–98.
Surakka, J., Romberg, A., Ruutiainen, J., Aunola, S., Virtanen, A., Karppi, S.-L., & Maentaka, K. (2004). Effects of aerobic and strength exercise on motor fatigue in men and women with multiple sclerosis: a randomized controlled trial. Clinical Rehabilitation, 18, 737–746.
† Sutherland, G., & Andersen, M. B. (2001). Exercise and multiple sclerosis: physiological, psychological, and quality of life issues. Journal of Sports Medicine and Physical Fitness, 41, 421–432.
Sutherland, G., Andersen, M. B., & Morris, T. (2005). Relaxation and health-related quality of life in multiple sclerosis: The example of autogenic training. Journal of Behavioral Medicine, 28(3), 249–256.
+ Sutherland, G., Andersen, M. B., & Stoove, M. A. (2001). Can Aerobic Exercise Training Affect Health-Related Quality of Life for People With Multiple Sclerosis? Journal of Sport and Exercise Psychology, 23, 122–135.
Tantucci, C., Massucci, M., Piperno, R., Betti, L., Grassi, V., & Sorbini, C. A. (1994). Control of breathing and respiratory muscle strength in patients with multiple sclerosis. Chest, 105, 1163–1170.
Tesar, N., Baumhackl, U., Kopp, M., & Gunther, V. (2003). Effects of psychological group therapy in patients with multiple sclerosis. Acta Neurologica Scandanavica, 107, 394–399.
† Thompson, A. J., Toosy, A. T., & Ciccarelli, O. (2010). Pharmacological management of symptoms in multiple sclerosis: current approaches and future directions. Lancet Neurology, 9, 1182–1199.
+ Turner, A. P., Kivlahan, D. R., & Haselkorn, J. K. (2009). Exercise and Quality of Life Among People With Multiple Sclerosis: Looking Beyond Physical Functioning to Mental Health and Participation in Life. Archives of Physical Medicine and Rehabilitation, 90, 420–428.
† Turner, A. P., Williams, R. M., Bowen, J. D., Kivlahan, D. R., & Haselkorn, J. K. (2006). Suicidal ideation in multiple sclerosis. Archives of Physical Medicine and Rehabilitation, 87, 1073–1078.
Uccelli, M. M., Mohr, L. M., Battaglia, M. A., Zagami, P., & Mohr, D. C. (2004). Peer support groups in multiple sclerosis: current effectiveness and future directions. Multiple Sclerosis, 10, 80–84.
van den Berg, M., Dawes, H., Wade, D. T., Newman, M., Burridge, J., Izadi, H., & Sackley, C. M. (2006). Treadmill training for individuals with multiple sclerosis: a pilot randomised trial. Journal of Neurology, Neurosurgery & Psychiatry, 77, 531–533.
+ Velikonja, O., Curic, K., Ozura, A., & Jazbec, S. S. (2010). Influence of sports climbing and yoga on spasticity, cognitive function, mood and fatigue in patients with multiple sclerosis. Clinical Neurology and Neurosurgery, 112, 597–601.
† Vickrey, B. G., Hays, R. D., Harooni, R., Myers, L. W., & Ellison, G. W. (1995). A health-related quality of life measure for multiple sclerosis. Quality of Life Research, 4(3), 187–206.
Walker, D. I., & Gonzalez, E. W. (2007). Review of intervention studies on depression in persons with multiple sclerosis. Issues in Mental Health Nursing, 28, 511–531.
† Ware, J.E. (1993). Measuring patients’ views: The optimum outcome measure: SF 36: A valid, reliable assessment of health from the patient’s point of view. British Medical Journal, 306, 1429-1430
Webster’s New World Dictionary, 2nd ed. (1982) Simon & Schuster, New York: NY.
West, S., King, V., Carey, T.S., Lohr, K.N., McKoy, N., Sutton, S., & Lux, L. (2002). Systems to rate the strength of scientific evidence. Evidence report/ technology assessment no.47 (Prepared by the Research Triangle Institute –University of North Carolina Evidence-Based Practice Center under contract no. 290-97-0011). AHRQ Publication No. 02-E016. Rockville, MD: Agency for Healthcare Research and Quality
White, A. T., Wilson, T. E., Davis, S. L., & Petajan, J. H. (2000). Effect of precooling on physical performance in multiple sclerosis. Multiple Sclerosis, 6, 176–180.
White, L. J., & Castellano, V. (2008). Exercise and Brain Health- Implications for Multiple Sclerosis; Part1- Neuronal Growth Factors. Sports Medicine, 38(2), 91–100.
† White, L. J., & Dressendorfer, R. H. (2004). Exercise and multiple sclerosis. Sports Medicine, 34(15), 1077–1100.
Wiles, C. M. (2008). Physiotherapy and related activities in multiple sclerosis. Multiple Sclerosis, 14, 863–871.
Wiles, C. M., Newcombe, R. G., Fuller, K. J., Shaw, S., Furnival-Doran, J., Pickersgill, T. P., & Morgan, A. (2001). Controlled randomized crossover trial of the effects of physiotherapy on mobility in chronic multiple sclerosis. Journal of Neurology, Neurosurgery & Psychiatry, 70, 174–179.
† University of California, Los Angeles. (1995). Mutiple Sclerosis Quality of Life (MS-QOL)-54 Instrument.