Speeding the Healing of Wounds in Old Age
Professor Jeroen Eyckmans recently received a $2 million grant from the Hevolution Foundation to address the urgent clinical challenge of repairing non-healing skin wounds in the elderly.
By Jim Cooney
Most medical and surgical treatments for wound care—such as the removal of dead tissue, cleaning and sterilization, closure with stitches or staples, and dressing—serve merely to facilitate living tissue’s own regeneration capacity. Tissue regeneration, a complex and intricate process that is still only partially understood, tends to serve us well in our youth but declines as we approach old age, and this decline can slow or fully impede the healing of wounds.
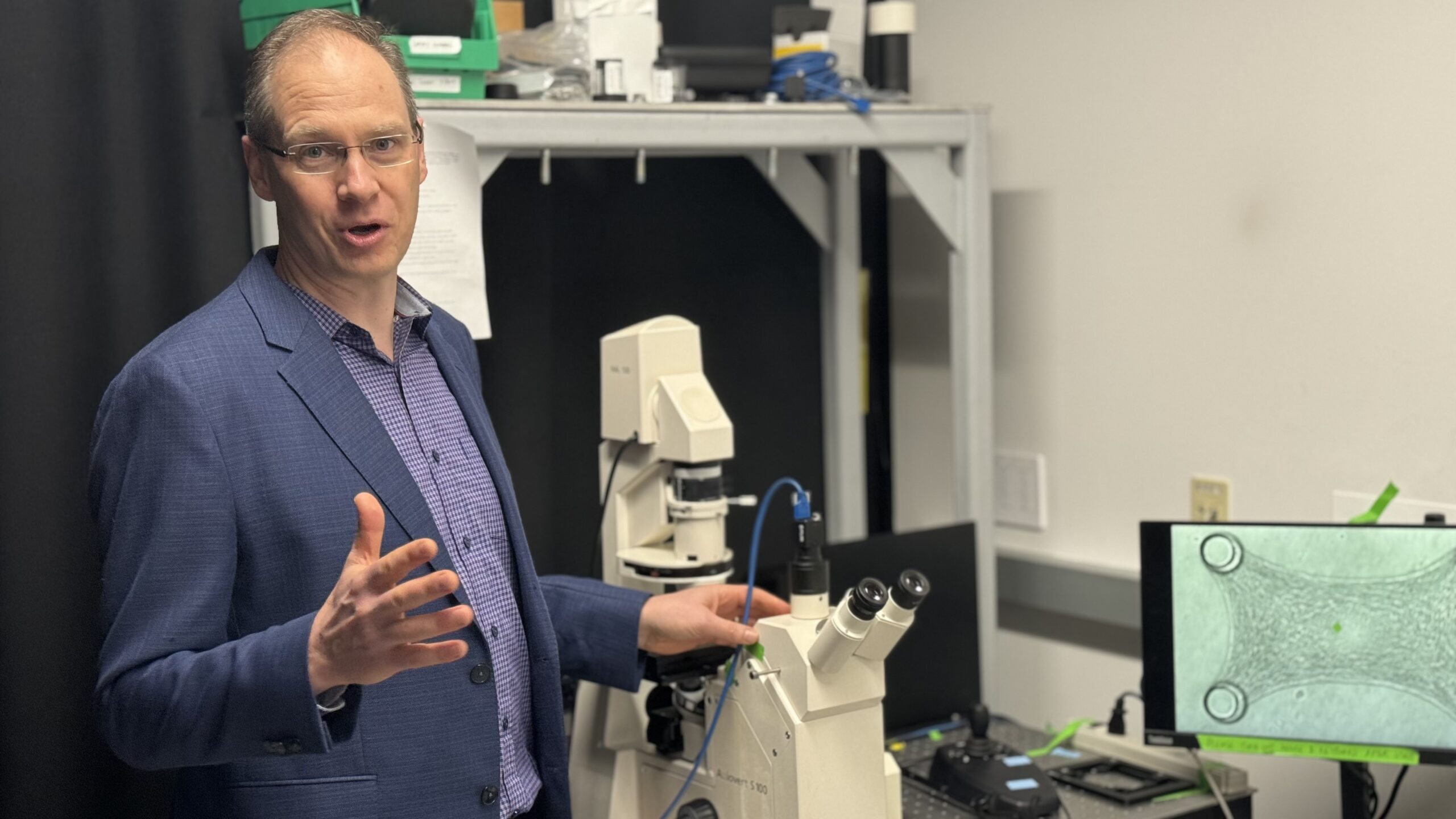
With an eye toward developing more advanced treatments, many scientists are attempting to better understand the wound healing process and what precisely underlies its decline in old age. Among them is Jeroen Eyckmans, a research assistant professor of biomedical engineering at Boston University (BU) and faculty affiliate of the Biological Design Center. With the support of a new $2 million grant from the Hevolution Foundation, which supports research and entrepreneurship in healthspan science, Eyckmans’ team will study impaired wound healing through a synthetic biology framework.
“When wounds don’t heal in a timely fashion,” says Eyckmans, “it can be very painful, hindering their ability to function at work or at home. There is also a high risk of infection which can lead to life-threatening sepsis. The last resort is sometimes amputation.” Currently in the U.S. it is estimated that impaired wound healing degrades quality of life for nearly 2.5 percent of the population and is suffered by 10.5 million Medicare beneficiaries. In other words, as the elderly population continues expanding with disproportionate speed, delayed wound healing represents both an urgent clinical and societal challenge.
Indeed, the mysteries behind wound healing have engaged researchers across many domains. Much of this research has focused on the activity of cells during the healing process. For instance, researchers may study how certain cells signal the start or the end of the inflammation phase of wound healing, and whether an age-related change in those cells causes a prolonged inflammation period that inhibits late-phase healing processes.
Eyckmans and his BU colleague Daniel Roh, an assistant professor of surgery at the Chobanian & Avedisian School of Medicine, are together taking a different approach to the study of wound healing. Rather than focusing mainly on the role of cells, Eyckmans and Roh will also be studying the role of the extracellular matrix. If we think of cells as the building blocks of life, we may think of the extracellular matrix as the scaffolding. In addition to providing structure and support to living tissues, the matrix helps facilitate cellular growth, movement, communication, and various other functions.
Not surprisingly, the extracellular matrix also plays a vital role in the wound healing process. “After the clotting phase, cells like fibroblasts move in and build what we call a ‘provisional matrix,’” says Eyckmans. “If you were to pull a bandage back, you might see in the wound bed a pinkish tissue that appears almost mucus-like in composition. That’s granulation tissue, and it provides a temporary or provisional matrix during wound healing. That’s what we’re looking for.”

How this provisional matrix changes throughout aging is one of the key research questions guiding Eyckmans’ and Roh’s team. Once they better understand these changes and their connection to delayed wound healing, the hope is that they can engineer a matrix in aged tissue that more closely resembles the matrix in young tissue, then observe whether this upgraded matrix helps to accelerate the healing process.
A second key question for this project involves studying how the provisional matrix interacts with cellular senescence–the process by which aging cells lose their ability to grow and divide. For a long time it was thought that the primary function of senescence was to prevent cells that had been damaged or corrupted by age from becoming cancerous. A study published in 2013, however, demonstrated that senescent cells also play an important role in wound healing.
Scientists know, for instance, that a brief inflammation of senescent cells followed by their removal seems necessary for advancing the healing process, but also that a prolonged inflammation of senescent cells leads to impaired healing. As we age, our proportion of senescent cells steadily increases, and scientists suspect this increase is another factor in delayed wound healing.
Eyckmans and Roh will use bioengineered model systems to better understand the extracellular matrix, senescent cells, and the “crosstalk” that occurs between them during the wound healing process. Eyckmans says this knowledge will enable the development of more sophisticated treatments. “Currently, most wound dressings and topical treatments attempt merely to reduce inflammation or speed collagen production,” says Eyckmans. “My hope is that our work will inform a new type of dressing that is focused on restoring the wound bed, making it function similarly to how it does in a young population.” This may mean, for instance, a dressing that releases a drug that removes senescent cells locally at a precise time in the healing process, Eyckmans says. “It may also mean engineering dressing material that more closely resembles the complexity of the wound bed itself, which contains over 300 extracellular proteins, each with a specific role.”