Recent Publications
Socio-demographic factors associated with hunger among food pantry users in Eastern Massachusetts
Check out this research article posted in the Journal of Nutritional Science by several members of BUSPH's Department of Community Health Sciences, including our very own, Jacey Greece!
Mothers Need a Continuous System of Care Even After Babies are Born
“COVID-19 and its unmasking of gender and racial inequities has driven home the urgency of the need to invest in the health and well-being of mothers beyond their reproductive health care, with laser-like attention to Black women.”
Read the article by Lois McCloskey, Ann Celi, Chloe Bird, Linda Goler Blount, and Judith Bernstien about why we need to focus on maternal health even after childbirth.
https://www.newsweek.com/opinion

Midwifery Webinar: An Evidence-Based Solution for Disrespect, Racism, and Other Challenges in Maternity Care
In light of high rates of maternal mortality, disrespect and racism in the United States, we discuss midwifery as an evidence-based solution and protective model to address the important challenges in women’s health care.
Join us on 4/29 from 1-2 PM EST. RSVP at https://hsph.me/midwiferywebinar.
Harvard & BU Midwifery Webinar April 29th Flyer
Featuring three renowned speakers:
- Ebony Marcelle, CNM, MS, FACNM, Director of Midwifery at Community of Hope
- Holly Powell Kennedy, PhD, CNM, FACNM, FAAN, midwifery researcher and Varney Professor of Midwifery at Yale School of Nursing
- Eugene R. Declercq, PhD, MBA, Professor of Community Health Sciences, Boston University School of Public Health
This webinar will be of special interest to midwives, public health or policy students, state Title V or other MCH practitioners, and those interested in equitable health care and maternal mortality.
You may now view the recording here https://www.youtube.com/watch?v=10NAag7w5h4
Expanding Postpartum Medicaid Benefits To Combat Maternal Mortality And Morbidity
MCH Research Fellow Gray Babbs shares research on how expanding postpartum medicaid benefits help to combat maternal mortality and morbidity.
https://www.healthaffairs.org/do/10.1377/hblog20210111.655056/full/
Massachusetts Public Health Association Virtual Breakfast Honoring Dr. Camara Jones September 18, 9:00am-10:00am
*Event Announcement*
Dr. Camara Jones September 18, 9:00am-10:00am
Youth Mental Health Access during COVID-19
Original Article by Michelle Samuels, July 15th 2020 - BUSPH "Youth Mental Health Access during COVID-19"
The coronavirus closed schools, contracted the economy, and is disproportionally devastating communities of color. In this pandemic and its aftermath, helping youths with mental health issues navigate decentralized services and stay out of the juvenile justice system may be more critical than ever, according to a new whitepaper co-authored by a School of Public Health researcher.
The paper outlines the work of the Health Law Advocates’ Mental Health Advocacy Program for Kids (MHAP for Kids) before and during COVID-19, and was highlighted at the Spring Meeting of the American Bar Association Commission on Homelessness and Poverty on June 6 as a model for best practice locally and nationally.
“Youth with unmet mental health needs including depression, anxiety, and trauma disproportionally end up in the court system, and MHAP for Kids has great potential to divert youth from court and help them get needed mental health services,” says Patricia Elliott, clinical assistant professor of community health sciences and the paper’s co-author with MHAP for Kids director Marisol Garcia.
“This is even more important now as the pandemic exacerbates existing conditions and introduces new stressors for families,” Elliott says.
In the paper, Elliott and Garcia outline the work of the program and how it has adapted for the new challenges of the COVID (and post-COVID) era.
“A fundamental reason why youth mental health services are difficult to access for families is that numerous different systems are supposed to provide such services. These systems include schools, clinicians, health insurance, state agencies, and the juvenile justice system,” they write.
MHAP for Kids provides free legal services and other help navigating and accessing these services for youth in income-eligible households in seven Massachusetts counties: Bristol, Essex, Hampden, Middlesex, Norfolk, Suffolk, and Worcester.
Elliott has been leading an independent evaluation of the program since it launched in two juvenile courts in 2015. In a paper published in 2017, Elliott and Emily Feinberg, associate professor of community health sciences, found that, out of 49 cases of youth court involvement for delinquency charges, the program avoided or shortened pre-trial detention for 16 youths, avoided adjudication due to competency concerns for 5, reduced sentences for 3, got treatment instead of detention for 1, and avoided Care and Protection cases for 12 youths by securing needed services. Elliott and Feinberg also recorded numerous other positive effects of the program, including reductions in conflict between youths and parents, less use of emergency mental health services, fewer inpatient hospitalizations or stays in emergency hospitals, increases in school attendance, and improved (parent-rated) mental health of youths and parents.
But in that 2017 evaluation, Elliott and Feinberg also found that 94 percent of the families served by MHAP for Kids reported experiencing challenges accessing mental health services for their children.
Now, COVID-19 is creating “new and more intensive barriers,” Elliott and Garcia write in the new paper.
These include school closures, which have interrupted specialized instruction and school-based counseling, while limited internet access and language barriers have made remote learning difficult for many families served by MHAP. All of these factors likely contribute to the worsening mental health of youths working with MHAP attorneys, and could have lifelong repercussions as these youths fall behind in education, Elliott and Garcia write.
To take on these issues, MHAP for Kids staff attorneys created a toolkit for other attorneys working with youth to advocate for their mental health needs during COVID, including sample letters and English- and Spanish-language forms for families to record issues. The American Bar Association Children’s Rights Committee has published the toolkit, available here.
Graph showing increase in youth of color served by the MHAP for Kids program compared to the pilot. Hispanic/Latinx youth make up the largest group of youths of color served, at 30%.
From “Advocating for Youth Access to Mental Health Services During a Pandemic” by Marisol Garcia and Patricia Elliott, presented at the American Bar Association Commission on Homelessness and Poverty Spring Meeting, June 6, 2020.Elliott and Garcia also outline how MHAP for Kids has adapted to better take on issues related to youths spending more time at home, economic challenges, and widening racial disparities during the pandemic. Much of this work was already underway before COVID, including efforts to help more youths of color—who are at particular risk for the “cradle to prison pipeline,” they write—and to place MHAP for Kids attorneys in counties with more low-income families. “Not by coincidence, the communities prioritized for assistance by MHAP for Kids using this approach have also been among the hardest hit by the pandemic,” the authors write.
“Having the program selected by the American Bar Association was a big honor,” Elliott says. “The results of the pilot evaluation were influential to the expansion of the program from two to seven counties within Massachusetts, and now we look forward to sharing the results of our current round of evaluation as more communities across the commonwealth and the country consider replication of the model to support youth and families.”
—Michelle Samuels
Massachusetts COVID-19 Perinatal Coalition
 https://www.massperinatal.org/
https://www.massperinatal.org/
Mission
To develop policy recommendations for equitable and evidence-based perinatal health care in the Commonwealth during the COVID-19 Pandemic, to promote systemic, consistent best practices and standards of care and support for pregnancy, childbirth, and postpartum, and to address racial inequities in perinatal outcomes.Situation
The current situation for birthing people in the Commonwealth is of the utmost concern. Due to the demands of the current pandemic on the health care system, the rapidly changing landscape of hospital policies, limited personal protective resources for providers and birthing people, and so much that is still unknown about transmission and treatment, the environment for birthing people and birthing people of color in particular has never been more precarious. In a landscape of changing and often inconsistently implemented policies, lack of adequate medical resources, and emergency demand on hospitals, the usual care and best practices for perinatal people is currently in constant flux or unable to be met. For brown and black childbearing people who are facing not only higher levels of infection, illness and death from COVID-19, but who also experience maternal mortality at a rate of 2 - 6 times that of their white counterparts, this is an urgent crisis that demands immediate attention. Additionally, 63% of all maternal deaths are preventable. Leadership is necessary to ensure that best practices and latest research are identified, consistently implemented and disparities eliminated for birthing people in the Commonwealth.Goals
Inform policymakers about the current needs for birthing people in the Commonwealth during COVID-19.Identify strategies and recommendations for achieving the best possible health outcomes for birthing people and babies.
Engage policymakers, health care providers, industry, and advocates to align efforts to uplift the needs of birthing people and end maternal health disparities in the Commonwealth and implement best health practices and standards of care for all birthing people during the COVID- 19 Pandemic with all due speed.
Resources and Reports
July 2020 "Giving Birth in a Pandemic"
Equity, Autonomy and Substance Use Disorder: Lifecourse Considerations for Pregnant and Parenting People

Wednesday, February 5th 2020
“Equity, Autonomy and Substance Use Disorder: Lifecourse Considerations for Pregnant and Parenting People”: co-hosted by Boston University and Harvard Schools of Public Health, Centers of Excellence in MCH, this webinar discussed the complex challenges and best practices for care of pregnant and parenting people with substance use disorder – especially after pregnancy and throughout the life course. Appropriate for public health practitioners, providers of all kinds, addiction specialists, maternal health advocates, substance use specialists, and policy-makers, alike.
Presentation recording (youtube): Recording - MCH and SUD Webinar - Feb 5 2020
Presentation slides (pdf): Slides - MCH and SUD Webinar Slide Deck- Feb. 5 2020
Q&A (pdf): Document - Webinar Q&A
Intrapartum Care and Experiences of Women with Midwives Versus Obstetricians in the Listening to Mothers in California Survey
MCH Faculty Eugene R. Declercq PhD, Candice Belanoff ScD, MPH, and Carol Sakala PhD, MSPH publish "Intrapartum Care and Experiences of Women with Midwives Versus Obstetricians in the Listening to Mothers in California Survey" in the Journal of Midwifery & Women's Health.
"Following the initial reporting of the Listening to Mothers in California survey in 2018, Drs. Declercq and Belanoff and I are involved in publishing several secondary analyses from this dataset." - Carol Sakala
Findings:
- Significant socioeconomic differences by type of intrapartum care provider, with women in California attended by midwives more likely to be well educated and privately insured than women attended by obstetricians.
- Women with midwife birth attendants were less likely to report experiencing various intrapartum medical interventions, less likely to experience pressure to have epidural analgesia, and more likely to report that staff encouraged the woman’s decision making.
- Adjusted odds ratios found that women with midwives were less likely to experience medical interventions, including attempted labor induction; labor augmentation; and use of pain medications, epidural analgesia, and intravenous fluids; and less likely to report pressure to have labor induction or epidural analgesia.
- Women cared for by midwives were more likely to experience any non pharmacologic pain relief measures and nitrous oxide and to agree that hospital staff encouraged their decision making.
READ: Intrapartum Care and Experiences of Women with Midwives Versus Obstetricians in the Listening to Mothers in California Survey
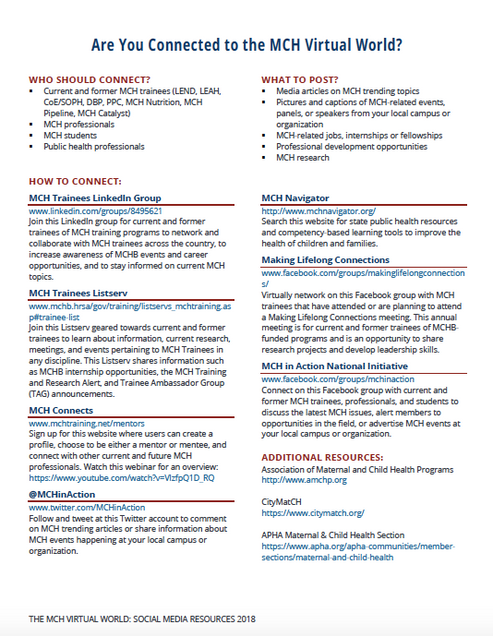
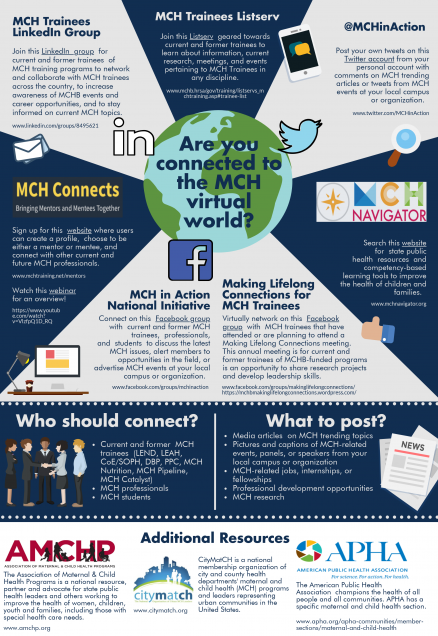
Are You Connected to the MCH Virtual World?
Connecting in the MCH Virtual World: a "how to" guide