The Ongoing Challenge of Substance Use and Its Consequences.
 A few months ago Massachusetts Governor Charlie Baker unveiled a proposed bill that aims to limit opioid prescriptions, triggered by alarm at the growing burden of opioid overdoses in the state. There is much that is commendable about the bill (and several controversial features). Centrally, though, it is encouraging to see the elevation of a public health problem to front-page attention by an administration that has focused on the issue for some time. Heartened by the growing attention to substance use and its health implications, I thought I would take a step back and summarize the burden of substance use that forms the backdrop for this latest piece of legislation.
A few months ago Massachusetts Governor Charlie Baker unveiled a proposed bill that aims to limit opioid prescriptions, triggered by alarm at the growing burden of opioid overdoses in the state. There is much that is commendable about the bill (and several controversial features). Centrally, though, it is encouraging to see the elevation of a public health problem to front-page attention by an administration that has focused on the issue for some time. Heartened by the growing attention to substance use and its health implications, I thought I would take a step back and summarize the burden of substance use that forms the backdrop for this latest piece of legislation.
Nearly 5 percent of total years of life lost globally are attributed to alcohol and illicit drug use. It is estimated that there are 185 million illicit drug users globally, and opioid dependence is the principal contributor to the burden of illicit drug dependence worldwide. The National Comorbidity Survey Replication estimates that about 4 percent of adults in the US have experienced a substance use disorder in the past year, or 1 in 25 adults. This is likely a substantial underestimate given the known high prevalence of substance use among homeless individuals and other groups who are missed in national surveys. Substance use disorders are associated with substantial morbidity and mortality, loss of economic productivity, unemployment, and intimate partner violence, and go hand in hand with psychiatric disorders and other comorbidities, including weight gain and obesity.
Substance use disorders are only the “tip of the iceberg” in terms of population health consequences of substance use. For example, in the absence of alcohol use disorder, binge drinking is a very common problem in the US that can lead to liver disease, injury, neurological damage, sexually transmitted diseases, and unintended pregnancy. Binge drinking is especially common in particular populations, for example among military personnel, where it has been associated with psychiatric comorbidity and risky behavior. Several of our faculty members have made substantial contributions to the field of substance use, and I will not here attempt a comprehensive list for fear of missing important work. Particularly relevant, however, Professor Richard Saitz has long noted the importance of thinking about unhealthy alcohol use as a frequently overlooked contributor to population morbidity.
Turning our attention to drug-related incidents, principally deaths that have informed much of the recent concern with opioids in the state and nationwide, colleagues and I recently reviewed the available literature on unintentional drug overdose globally. The review concluded unequivocally that globally overdose is on the rise, particularly in rural areas and especially from prescription opioids. From 1999 to 2008, hospitalization rates for overdoses in the US increased by 55 percent, costing about $737 million in 2008, a figure that is undoubtedly dwarfed today. The figure below summarizes data that has long made clear the dramatic burden of mortality linked to substance use, showing that drug-related deaths have exceeded motor vehicle deaths in this country for nearly a decade.
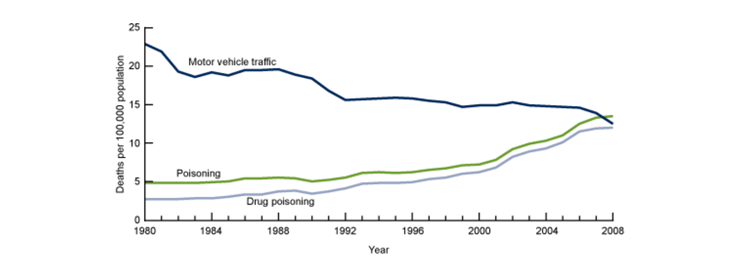
Motor vehicle accident deaths have declined while drug overdose deaths have increased in the past thirty years. M Warner, LH Chen, DM Makuc, RN Anderson, AM Miniño. Drug poisoning deaths in the United States, 1980–2008. NCHS Data Brief. 2011;81(22):1–8. http://www.cdc.gov/nchs/data/databriefs/db81.htm
As the availability of prescription opioids has increased across the US, illicit drug use has gone down in many areas. However, one unexpected consequence of this shift is that many individuals who would not be likely to use heroin otherwise are introduced to opioids through prescription opioids, and then later turn to heroin as their tolerance for the substance increases or they no longer have access to the medication. One result of this shift is that heroin use is actually starting to increase again, especially among affluent people living in the suburbs, a very different group from those generalized as having heroin addictions in decades past.
Importantly, stricter policing practices, not atypically linked to the rise in drug-related overdoses, can themselves contribute to increase drug-related deaths, principally as drug-users move underground and witnesses to overdoses are reluctant to call for help. Perhaps optimistically, the growing burden of drug-related overdose has made it abundantly clear that drug-related overdose is no longer simply labeled a law enforcement or public safety issue, but a public health issue. One major aspect of public health relevance is that overdose is usually preventable, and individuals rarely overdose alone, providing a unique opportunity to avoid death, particularly for those witnessing an overdose. Provision of the opioid antagonist naloxone to drug users, a practice that is being implemented in many areas, is one example of a way to potentially stop the harm of an overdose before it leads to death. Hearteningly, some innovative efforts across the US, including several here in Massachusetts, are taking the initiative to move beyond thinking of substance use as a legal issue to thinking of it as a public health issue.
A few weeks ago, a study published in the Proceedings of the National Academy of Sciences, brought home the consequences of drug use simply and effectively showing that if the death rate among those aged 45 to 54 had continued to decline the way it had between 1979 and 1998, we would have avoided half a million deaths between 1999 and 2013, comparable to the number of lives lost to AIDS in the US; I referred to this paper in last week’s Dean’s Note.
Once again on the “tip of the iceberg,” mortality is far from the only consequence of drug use. Other associated outcomes include hospitalization cost and lost work productivity. Additionally, consequences of nonfatal overdose among victims include cardiac and muscular problems, cognitive impairment, renal failure, and other injuries. Moreover, following the lifecourse paradigm, effects of substance use can spill over from generation to generation; maternal smoking during pregnancy is associated with low birth weight, among other effects in offspring, and using alcohol and other substances during pregnancy is associated with a myriad of outcomes, including pre-term birth, placental abruption, neonatal withdrawal, and cognitive deficits.
The growing focus on non-medical opioid overdose state-wide and nationwide is welcome, but this approach deals only with a small part of a much larger problem with the use of substances worldwide. The burden of substance use is very much a chronic challenge to population health that has long been underappreciated and on the fringes of mainstream public health. Unfortunately, this marginalization is accompanied by substantial shortage in opportunities for treatment for those with substance dependence, attendant unmet need, and an even deeper paucity of engagement around prevention of substance use and misuse. The recent attention to the issue is an important, if small, turn in the right direction.
I hope everyone has a terrific week. Until next week.
Warm regards,
Sandro
Sandro Galea, MD, DrPH
Dean and Professor, Boston University School of Public Health
Twitter: @sandrogalea
Acknowledgement: I am grateful for the contributions of Laura Sampson to this Dean’s Note.
Previous Dean’s Notes are archived at: https://www.bu.edu/sph/category/news/deans-notes/