Researchers Awarded $26.56 Million Grant for Brain Aging Program.
Since 1976, the Boston University-based Framingham Heart Study (FHS)—the longest running multi-generational epidemiological study in the world, begun in 1948—has followed participants for incident dementia. The findings have helped to analyze the differences between normal, age-related changes in thinking and disease-related pathological alterations. In addition, the inclusion of many of the original participants’ children and grandchildren has also provided an opportunity to explore genetic factors related to Alzheimer’s disease (AD) and vascular dementia.
Now, thanks to a five-year, $26.56 million grant from the National Institutes of Health, a new program called the Framingham Heart Study Brain Aging Program (FHS-BAP) will continue the surveillance and evaluation of FHS participants for dementia (including cognitive assessments and brain imaging) and invigorate the FHS brain donation program and brain bank. The program will also establish a platform to promote data sharing that will accelerate AD research using FHS data and conduct three interrelated projects using FHS data and specimen resources.
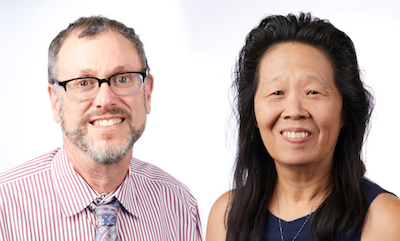
Lindsay Farrer, chief of biomedical genetics at the School of Medicine and professor of biostatistics and epidemiology at the School of Public Health, is one of two principal investigators of the award and will lead the research. “The primary goal of this new program is to continue dementia surveillance, bring added resources to the brain donation program including neuropathological examination to identify new and expand on known AD-related genetic and other risk factors and biomarkers and to pursue innovative research about the vascular and inflammatory basis of AD,” he explains.
The FHS-BAP will feature three inter-related projects that focus on vascular and inflammatory contributors to AD. One project will identify factors that are associated with AD risk and resilience using longitudinal analyses of FHS data including various genetic, clinical, imaging, lifestyle and other traits. A second project will investigate the link between AD genetic vulnerabilities and chronic inflammation. A third project will study the impact of variants in genes affecting immune function on AD-related brain changes and cognitive performance. All of the projects will leverage the unique features of this family-based cohort and up to 70 years of follow-up data collected from study participants.
The other principal investigator, Rhoda Au, professor of anatomy & neurobiology, and neurology at the School of Medicine and of epidemiology at the School of Public Health, will coordinate research participant engagement in this program. “FHS-BAP investigators will apply inter-disciplinary approaches that maximize use of a wide array of clinical, lifestyle, biomarker and ‘omic information collected from three generations of FHS participants over the course of their adult lives to develop strategies that preserve cognition and memory and to identify novel therapeutic targets,” she says.
Finally, “this program will promote using FHS-BAP data, especially by early-stage and investigators nor currently working in the AD field using a pilot projects program and through enhanced and proactive data sharing efforts,” says Farrer, who is also a BU Distinguished professor of genetics as well as a professor of medicine, neurology, and ophthalmology at the School of Medicine.
Farrer’s research has led to more than 450 publications on genetic risk factors for several familial neurodegenerative and other chronic diseases. In collaboration with other laboratories worldwide, his group has identified genes and delineated mechanisms causing a variety of rare and common disorders including AD, age-related macular degeneration, substance use disorders, Wilson disease, Machado-Joseph disease, Waardenburg syndrome, and hypertension.
Au has been involved in FHS research related to cognitive aging and preclinical/clinical dementia since 1990. The limits of standard neuropsychological testing led her to apply the Boston Process Approach (BPA) to increase the sensitivity of these tests. The BPA includes tracking error and extraneous responses and she has exponentially expanded the scientific potential of the BPA approach by introducing digital technologies to detect changes in cognition much more effectively than traditional paper-pencil tests. FHS is the first to apply the BPA method to epidemiologic research. She is currently focused on building multi-sector ecosystems to enable solutions for chronic disease prevention generally and optimizing brain health specifically and to move the primary focus of health technologies from precision medicine to a broader emphasis on precision health.
The FHS has had a major impact on public health by establishing links between cholesterol and heart disease, blood pressure and stroke, as well as precursors to a variety of other diseases associated with aging.