Where You Live Determines Risk of Severe Pregnancy, Postpartum Complications.
Where You Live Determines Risk of Severe Pregnancy, Postpartum Complications
A new study found that Washington, DC had the highest rate of severe maternal morbidity in the country—nearly three times as high as Utah, the state with the lowest rate.
The chance of experiencing life-threating complications from pregnancy, childbirth, or the postpartum period may depend on where you live in the United States, according to a new study led by a School of Public Health researcher.
Published in the journal Obstetrics & Gynecology, the study examined maternal health outcomes among Medicaid insurance recipients and found that rates of severe maternal morbidity (SMM), or “near miss” deaths, varied substantially by state and by race/ethnicity.
Across the country, SMM rates were highest in Washington, DC, at 200 cases per 10,000 live births—nearly three times as high as Utah, the state with the lowest SMM rate, at 80 cases per 10,000 live births. In a subsample of 27 states and Washington, DC with adequate race and ethnicity data,the researchers found that the rate of SMM among Black birthing people was nearly twice as high as the rate for White birthing people.
Prior research has shown that maternal morbidity and mortality rates rose sharply during the COVID-19 pandemic. The team hopes these new findings will inform tailored,state-levelinterventions to address these SMM rates and the racialinequities in SMM.
“It is important for policymakers and clinicians to understand the geographic and demographic differences in rates of severe maternal morbidity among Medicaid patients so that resources and interventions can be targeted to maximize reductions in both overall morbidity and disparities in morbidity between groups,” says study senior author Sarah Gordon, assistant professor of health law, policy & management.
For the study, Gordon and colleagues from SPH, the University of Michigan, Columbia Mailman School of Public Health, and the University of Minnesota School of Public Healthexamined nearly five million live births among Medicaid enrollees from 2016 to 2018. They identified adverse maternal health outcomes, overall and by state, that occurred within six weeks of delivery. The team utilized a novel data source called the Transformed Medicaid Statistical Information System (T-MSIS), which is a national database of healthcare claims for Medicaid enrollees that wasprovided by the Centers for Medicare and Medicaid Services (CMS).
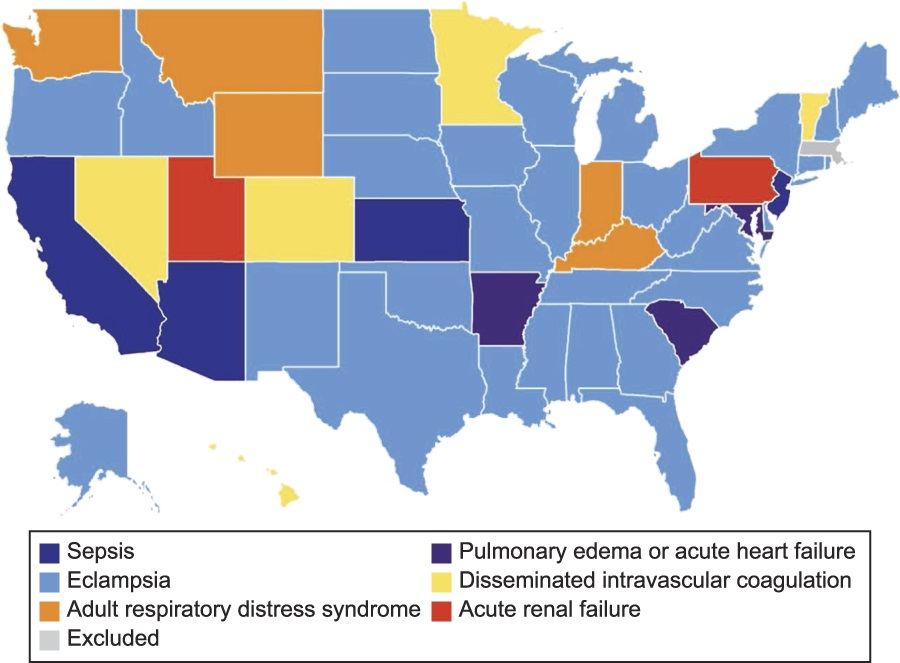
In addition to DC, the top five states with the highest SMM rates were California, Nevada, New Jersey, and New York, while Maryland, Rhode Island, Nebraska, and New Hampshire joined Utah as the states with the lowest rates.
However, these state-level complications varied when considering race. Among Black Medicaid patients, the highest SMM rates were Alaska, New York, and New Jersey, and the lowest rates were in New Mexico, North Dakota, and Utah. Among White Medicaid patients, the highest SMM rates were in California, West Virginia, and South Carolina, and the lowest rates were in Utah, North Dakota, and Maine.
Of note, the study is the first to generate national data on severe maternal mortality among Medicaid enrollees. Researchers often have difficulty accessing this type of federal data due to limited technical resources, compliance issues, or cost. The team utilized the expertise of data analysts and developers at SPH’s Biostatistics and Epidemiology Data Analytics Center (BEDAC), who are in the process of developing a novel digital warehouse that will store and manage massive amounts of CMS data to make this information more accessible and scalable for BU researchers.
“Our goal is to provide a cost-effective and user-friendly resource that meets the compliance needs of CMS data, and optimizes an environment that will make project teams more efficient in utilizing complex and high-impact Medicare and Medicaid data,” says Joseph Palmisano, associate director of data management for BEDAC.
“These data represent a significant improvement in data quality about Medicaid beneficiaries, enabling studies like ours and others that seek to study a program that covers over 90 million low-income people and serves as the primary payer for births, children, mental health care, and long-term care in the United States,” Gordon says.
The lead author of the study was Lindsay Admon, associate director of the Health Policy & Economics Pathway of Excellence at the University of Michigan Medical School. At SPH, the study was coauthored by Eugene Declercq, professor of community health sciences, and doctoral student Samantha Auty.