Young Adults Are Dying Earlier Than Expected.

Young Adults Are Dying Earlier Than Expected
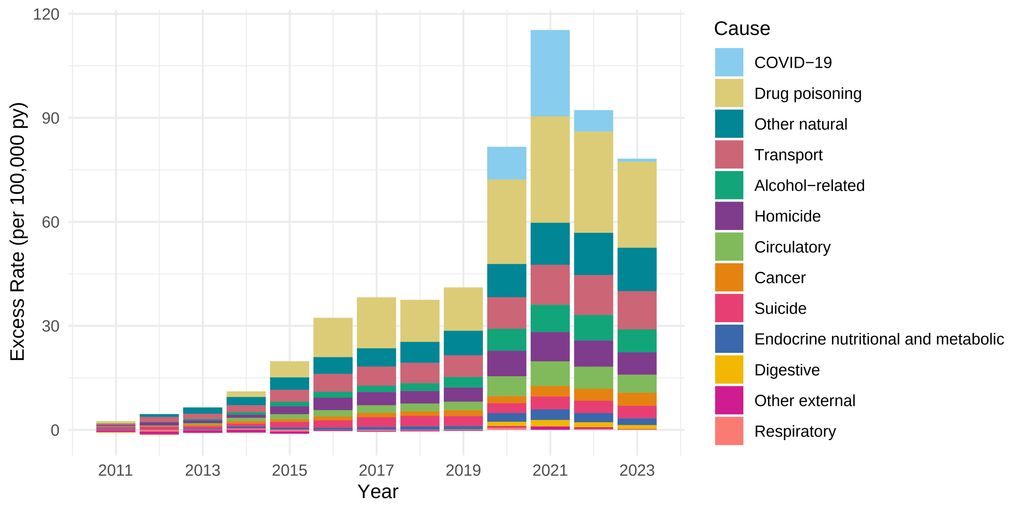
Mortality among adults ages 25-44 began rising at an alarming rate in 2011 and accelerated even more during the COVID-19 pandemic. This spike was largely driven by substance misuse, followed by poor nutrition and transportation accidents.
Death rates for early adults, defined as adults aged 25-44, rose sharply during the COVID-19 pandemic and remain higher than expected post-pandemic, according to a new study led by researchers at the School of Public Health and the University of Minnesota.
Published in JAMA Network Open, the study found that heightened death rates during the COVID-19 pandemic intensified an already negative trend for early adults, which began around 2010. As a result, early adult death rates in 2023 were about 70 percent higher than they might have been if death rates had not begun to rise about a decade before the pandemic.
“Our findings underscore the urgent need for comprehensive policies to address the structural factors driving worsening health among recent generations of young adults,” says study senior author Andrew Stokes, associate professor of global health.
For the study, the researchers analyzed nearly 3.4 million deaths among early adults in the US between 1999-2023. For early adults, there was a large jump in the death rate between 2019 and 2021, which are considered the core pandemic years. The death rate for this age group was nearly 35 percent higher than expected in 2019, and nearly three times higher in 2021 than what it had been in 2019. By 2023, the death rate remained nearly 20 percent higher than in 2019, and 70 percent higher than it would have been had mortality trends prior to 2011 continued.
Drug-related deaths were the single largest cause of 2023 excess mortality, compared with the mortality that would have been expected had earlier trends continued. Other important contributing factors were a variety of natural causes, including cardiometabolic and nutritional causes such as heart disease and diabetes, and a variety of other external causes, including transportation-related deaths.
“The rise in opiate deaths has been devastating for Americans in early and middle adulthood,” says study lead author Elizabeth Wrigley-Field, associate professor in the University of Minnesota College of Liberal Arts and Institute for Social Research and Data Innovation. “What we didn’t expect is how many different causes of death have really grown for these early adults. It’s drug and alcohol deaths, but it’s also car collisions, it’s circulatory and metabolic diseases—causes that are very different from each other. That tells us this isn’t one simple problem to fix, but something broader.”
The rise in deaths among early adults is especially concerning because it portends that this mortality crisis may worsen as this population ages.
“There’s an urgent need to address the root causes of these excess deaths, such as transportation safety, alcohol-related harm, and the food environment, among other factors,” says study coauthor Rafeya Raquib, research fellow in the Department of Global Health.
Such solutions may include expanding access to nutritious foods, strengthening social services and increasing regulation of industries that affect public health, says Stokes. In future research, the team will explore ongoing consequences of the COVID-19 pandemic and the trends that were already in place when it began.
Importantly, these findings contradict how society tends to view death—as a tragedy that primarily befalls older adults, says Deborah Carr, A&S Distinguished Professor in the Department of Sociology at BU’s College of Arts & Sciences, and director of the Center for Innovation in Social Science. Carr was not involved with the study but is a life-course sociologist who has written extensively on inequality in old age, death and dying, bereavement, and family relationships over the life course.
The findings underscore the need for researchers to continue examining the long-term consequences of the COVID-19 pandemic—as well as the health trends that existed prior to the pandemic. “Of the more than 3 million deaths each year in the U.S. about three-quarters are to people ages 65+ and older. But youthful deaths are often ignored,” Carr says. The alarming increase in deaths among young people ages 25-44 “means that young children are losing their parents, older adults are losing the grown children who are their caregivers, and employers are losing workers in their prime years. At this moment when support for health research is being threatened, we need studies like this to show us who is at risk of premature death, why it’s happening, and what to do about it.”