More than half of the servicepeople who fought in Iraq or Afghanistan have service-related physical or mental health problems, and one in two veterans knows a fellow service member who has attempted or committed suicide, according to a poll conducted by the Washington Post and the Kaiser Family Foundation. The same survey found that more than one million veterans suffer from key indicators of post-traumatic stress disorder (PTSD).
Dozens of BU scientists on the Charles River and the Medical Campuses are doing work that could improve the lives of many of the 2.6 million service members who fought in Iraq and Afghanistan: research on wound healing, pulmonary function, amputation repair, intimate partner violence and eating disorders among female veterans, and various aspects and consequences of PTSD and traumatic brain injury. And the BU community has dozens more who are social workers, educators, and clinical care providers working closely with veterans and their families.
In light of the still largely unmet health needs of US service members and the breadth of expertise at BU, the School of Medicine recently launched the Center for Military and Post Deployment Health, which will coordinate the University’s many and various military-focused research and service projects.
The center displayed some of its expertise November 3, 2015, when MED hosted its fourth annual Joining Forces Conference, where researchers talked about their groundbreaking work. The Joining Forces initiative was started in 2011 by Michelle Obama and Jill Biden, who collaborated with the Association of American Medical Colleges to encourage a commitment by medical workers to meet the health care needs of military veterans and their families. The BU Medical Campus was one of the original participants in the program. In 2015, more than 100 medical schools sponsored events.
Anna Hohler (CAS’98, MED’98), a MED associate professor of neurology, assistant dean of clinical and strategic affiliations, and director of the new center, says MED’s Joining Forces Conferences highlight the research and education happening on the Medical Campus through collaborations with VA Healthcare centers and demonstrate the University’s potential to contribute to advances in military health care.
Karen Antman, MED dean and provost of the Medical Campus, has a long-standing interest in the health of people serving in the military. In 2014 she organized a roundtable discussion among faculty and staff from both campuses, inviting medical researchers, social workers, and ROTC leaders to talk about creating a permanent institution to coordinate interdisciplinary research and programming on military medical issues.
“We have been working on establishing a center for military health for more than a year,” says Antman. “Our faculty have substantial expertise in trauma, PTSD, traumatic brain injury, environmental exposures (Gulf War syndrome, agent orange), blast ear injuries, suicide, and gender issues in deployment health, and are clearly committed to serving active duty and veteran military families. We have three affiliated VA hospitals, in Boston and Bedford, Mass., and in Manchester, N.H. Of all of our many campus-wide planning workshops, the one on military medicine attracted the most faculty, and enthusiasm.”
The roundtable participants discussed several possible projects that could benefit from such a center.
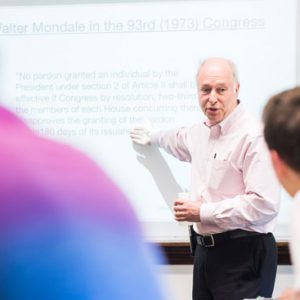
“We talked about developing curriculum for medical students, dental students, social work students, and graduate medical students,” says Hohler, who served in the Army for eight years, reaching the rank of major. “We also talked about how we might integrate some of that learning into the ROTC curriculum, so ROTC students could learn about post-traumatic stress disorder and traumatic brain injury.”
First Step: Developing a Database
Hohler says medical students currently learn about traumatic brain injury in a Human Behavior in Medicine course taught by Douglas Hughes, MED’s Ramsey Professor of Theory and Practice and associate dean of academic affairs, and they learn about PTSD in the psychiatry session of the Disease and Therapy Course directed by John Otis, a MED associate professor of psychiatry.
She says that as center assistant director, Monica Parker-James is developing a database of all MED military-related work. “That’s the first step in a cohesive approach to our research platform,” says Hohler. “We also have launched our website, which will house all of the Joining Forces Conference programming and provide information about research projects, educational initiatives, and clinical collaborations.” Hohler and Parker-James, who is also manager of clinical and strategic affiliations in MED’s academic affairs office, will organize working groups for each of these focus areas.
Hohler completed a neurology internship and residency at Madigan Army Medical Center in Tacoma, Wash., where she subsequently was chief of the neurology clinic and director of the neurology residency program. Her research interests include symptomatic predictors of Parkinson’s disease and novel medication and surgical therapies for Parkinson’s patients. She is the recipient of numerous awards, including the Army Achievement and Commendation Medals and two Meritorious Service Medals for excellence in clinical and teaching skills while on active duty. She also received MED’s Stanley L. Robbins Award for Excellence in Teaching and several neurology teaching awards, two from the American Academy of Neurology.
“We are delighted that Dr. Hohler accepted the responsibility of leading the center,” says Antman. “She is former military and an outstanding leader.”





































As a BU alumnus, I am very gratified to learn about this endeavor on behalf of our veterans. Given the decidedly leftist slant of most campuses today- including BU- I was surprised that such a project was not thwarted by the knee jerk anti military crowd there.
Thank you Boston University for this effort. A bit late but better than never. I receive excellent medical care from the Boston VA system and especially from those who work there. Would have to believe the care will improve via the research and assistance from Boston University. Ideally, the program could expand into other VA’s around the country.
War sucks but coming home with no resources to deal with the after effects is much worse.