Antibiotics are a cornerstone of modern medicine, saving hundreds of millions of lives around the world since the discovery of penicillin in 1928. Today, however, emerging antibiotic-resistant superbugs are outstripping the supply of new drugs to treat deadly bacterial infections. The lack of financial reward has led the pharmaceutical industry to all but abandon the development of new antibiotics. Both the Centers for Disease Control and Prevention (CDC) and the World Health Organization have identified antibiotic resistance as one of the greatest threats to public health worldwide.
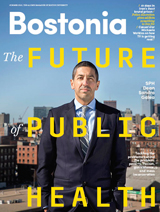
As part of its sweeping effort to tackle the problem, the United States Department of Health and Human Services (HHS) announced on July 28, 2016, that it has selected the School of Law—and Kevin Outterson, a BU professor of law—to lead a novel $350 million trans-Atlantic public-private partnership to spur the preclinical development of new antibiotics and antimicrobial rapid diagnostics and vaccines. The partnership is called Combating Antibiotic-Resistant Bacteria Biopharmaceutical Accelerator, or CARB-X.
“The grant to establish the CARB-X project, with Kevin Outterson of the School of Law as executive director, is a major milestone for Boston University,” says BU President Robert A. Brown. “That the leadership for this collaboration among very distinguished public and private entities comes from Boston University is testament to our range and depth as a research university. Most of us understand the arms race that is ongoing between the natural evolution of bacteria harmful to humans and our development of the drugs that combat them. The CARB-X project will accelerate drug development in this critical race with nature.”
“Anything that reduces the human burden of resistant bacterial disease is on our table,” says Outterson, who is a leading expert on the economic and legal framework needed to refuel the antibiotics pipeline and will serve as CARB-X principal investigator as well as executive director. “We’re looking for game-changing products that will make dramatic improvements in human health—not incremental change. We’re going to spend this money on the areas of greatest health need, focusing on things that major pharmaceutical companies have abandoned.”
Joining Outterson’s executive team at BU will be two physician-scientists with decades of experience in antibiotic drug development. John H. Rex, senior vice president and chief strategy officer for AstraZeneca Pharmaceuticals’ Infection Business Unit, will serve as chief strategy officer; and Barry I. Eisenstein, a distinguished physician in antimicrobials at Merck (previously at Cubist Pharmaceuticals), will begin working with CARB-X as chair of the Scientific Advisory Board after he retires from Merck in January 2017. Eisenstein helped lead the US Food and Drug Administration (FDA)–approval process for Cubicin (daptomycin), among the most successful antibiotics developed for life-threatening infections caused by drug-resistant bacteria, like MRSA, in the last 25 years.
“Kevin has brought together a team of interdisciplinary researchers and policy advocates to tackle this very complex global public health problem,” says LAW Dean Maureen O’Rourke. “He brings a deep understanding of the economic, environmental, and regulatory policies that are among the factors underlying the problem.”
The Biomedical Advanced Research and Development Authority (BARDA), within HHS, will provide $30 million in grants to CARB-X during the first year and up to $250 million over five years. The Antimicrobial Resistance Centre, a British government–sponsored public-private initiative that supports the development of new antibiotics and diagnostics, will provide an additional $14 million the first year and up to $100 million over five years. Another British partner, Wellcome Trust, a London-based global charitable foundation that supports biomedical research, will contribute further funding. After a strategic review last year, Wellcome made drug-resistant infections one of its priority areas. CARB-X is one component of that work and Wellcome says it can’t be more specific about funding until it finalizes its overall portfolio in that area, which it hopes to do later this year.

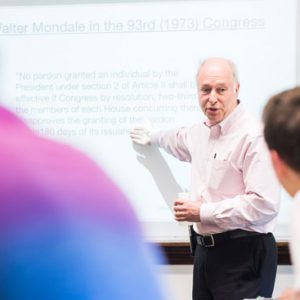
Outterson turned to John H. Rex, a senior vice president at AstraZeneca Pharmaceuticals and a leader in antibiotic drug development, for help in putting together the CARB-X team that won the $350 million grant. Photo by Cydney Scott
“The bulk of the money will go to research labs and small companies developing innovative products all over the world,” says Outterson, who is LAW’s N. Neal Pike Scholar in Health and Disability Law and codirector of the health law program. “We will fund the best science, wherever found. The goal is to invest money so that the products society needs will be ready in a decade. This is a social investment. We’re trying to build a fire station before the buildings catch on fire.”
CARB-X, which grew out of President Obama’s 2015 Combating Antibiotic-Resistant Bacteria (CARB) initiative, comes amid a global consensus that urgent action is needed. “The establishment of CARB-X is a watershed moment,” says Richard Hatchett, BARDA’s acting director. “Governments, academia, industry, and nongovernmental organizations have come together to operate under a common strategic framework to tackle a monumental public health threat of our time.”
Another CARB-X partner is the NIH’s National Institute of Allergy and Infectious Diseases (NIAID). In a July 28 telephone briefing with reporters, NIAID director Anthony S. Fauci said that his agency’s support of CARB-X reflects its steadily growing commitment to basic research into antimicrobial resistance as well as to the development of new antibiotics and other tools to address the problem. CARB-X, said Fauci, “consolidates antimicrobial research strategy into one package.”
The Broad Institute at Harvard and MIT is another CARB-X partner. Deborah Hung, co-director of the Broad’s infectious disease program, recently created the Collaborative Hub for Early Antibiotic Discovery, an interdisciplinary center whose researchers will share with product developers their expertise in medicinal chemistry, analytical screening, pharmacokinetics, and other areas of early-stage drug development.
“The reason that this [CARB-X] is such a big deal is that we have essentially not had a new class of antibiotics for decades,” says Hung, an associate professor of microbiology and immunobiology at Harvard Medical School. Because of what is viewed as the broken business model for new antibiotics, and the scientific and regulatory barriers, says Hung, “big pharma and everyone else has gotten out. So here is a new model for antibiotic discovery and development. It’s not going to solve all the problems, but it’s going to solve a piece of it.”
CARB-X expects to build a portfolio of more than 20 high-quality antimicrobial products—drugs as well as rapid diagnostics and vaccines that will cut down on the misuse of antibiotics. That is many more products than a company can normally take on, says BARDA’s deputy director, Joe Larsen, who points out that 80 to 90 percent of drugs fail during the early stages of development, “so our chances of getting innovative products into clinical testing within five years are higher than normal. By working together, we can accelerate at least two products to reach clinical testing within five years.”
In addition to awarding grants to product developers, CARB-X partners—a group that includes two nonprofit life sciences accelerators, one in Massachusetts, the other in San Francisco—will pool their broad scientific, technical, business, and legal expertise to help grantees navigate the maze of regulatory steps, studies, and data collection required for new drugs and other products to gain approval from the FDA. At that point, Outterson says, the new antibiotics and other products will be in a position to attract private investment to continue advancing to the marketplace.
The business support is crucial, says Michael Kurilla, who directs NIAID’s Office of Biodefense Research Resources and Translational Research and is a member of the CARB-X executive team. “Many promising therapeutics fail, as a result of business deficiencies,” he says. “A number of start-ups are unsuccessful because their corporate structure is not organized or managed appropriately for the long-term commitment of drug development that would instill confidence for future support by investors.”
Among the things that distinguish CARB-X from previous efforts to refuel the antibiotic pipeline, Kurilla says, is that it is being led, not by a scientist, but by a law professor. “Kevin brings to this enterprise a broad overview of the big picture associated with all of the issues surrounding the market failure of antibiotic development,” Kurilla says. “As a lawyer who understands the economics involved and a member of several global advisory groups working on antibiotic resistance, he is a tremendous asset. We like to think that drug approval is determined by the scientific, technical, and medical aspects of just the product, but the reality is that the management of the business itself has to be successful for promising candidates to succeed.”
Other CARB-X partners include RTI International (RTI), the Massachusetts Biotechnology Council, and the California Life Sciences Institute. RTI, a global research support organization based in North Carolina’s Research Triangle Park, will provide research support for product developers. “Small companies often lack experience with contract research organizations and the protocols necessary to move a compound toward human clinical trials,” says Outterson. “RTI will fill that vital need.” RTI will also build and run the computing systems to identify, track, and monitor all research programs and lead in the evaluation process of new products.
The Cambridge-based Massachusetts Biotechnology Council and the California Life Sciences Institute in San Francisco will both provide mentoring and business support to CARB-X innovators, so that their products will merit the private or public investment needed to advance to approval by the FDA, the UK’s European Medicines Agency, and other drug regulatory authorities.
At the outset, CARB-X will focus on Gram-negative bacteria that the CDC has classified as “urgent” or “serious” threats and which are increasingly resistant to most available antibiotics. These include:
- Carbapenem-resistant Enterobacteriaceae (CRE), like E.coli, which usually cause infections in patients in health care settings. One report says that CRE infections can contribute to death in up to 50 percent of patients who become infected, according to the CDC.
- Clostridium difficile or C. diff, which can cause life-threatening diarrhea and occurs mostly in people who have had both recent medical care and antibiotics. C. diff caused nearly half a million infections among patients in a single year, according to a 2015 CDC study, and an estimated 15,000 deaths.
- Neisseria gonorrhoeae, which causes gonorrhea, a sexually transmitted disease that is increasingly becoming resistant to antibiotics.
Decisions on the most promising products to fund will be made by the Scientific Advisory Board, which will include independent scientists from all over the world, with input from funders.




































Related Stories
LAW-based CARB-X Awards $24 Million for Superbug Antibiotics
Wellcome Trust gives $155M for nonprofit’s work on “huge global challenge”
BU-Based CARB-X Antimicrobial Partnership Gets Another $50 Million Plus
Gates Foundation, UK government contributions push CARB-X funding to more than $500 million
Preventing an Antibiotic Apocalypse
LAW prof: universities key to fixing broken drug innovation business model
Post Your Comment