Using Light to Monitor Blood Pressure and Track Cancer Treatment Progress

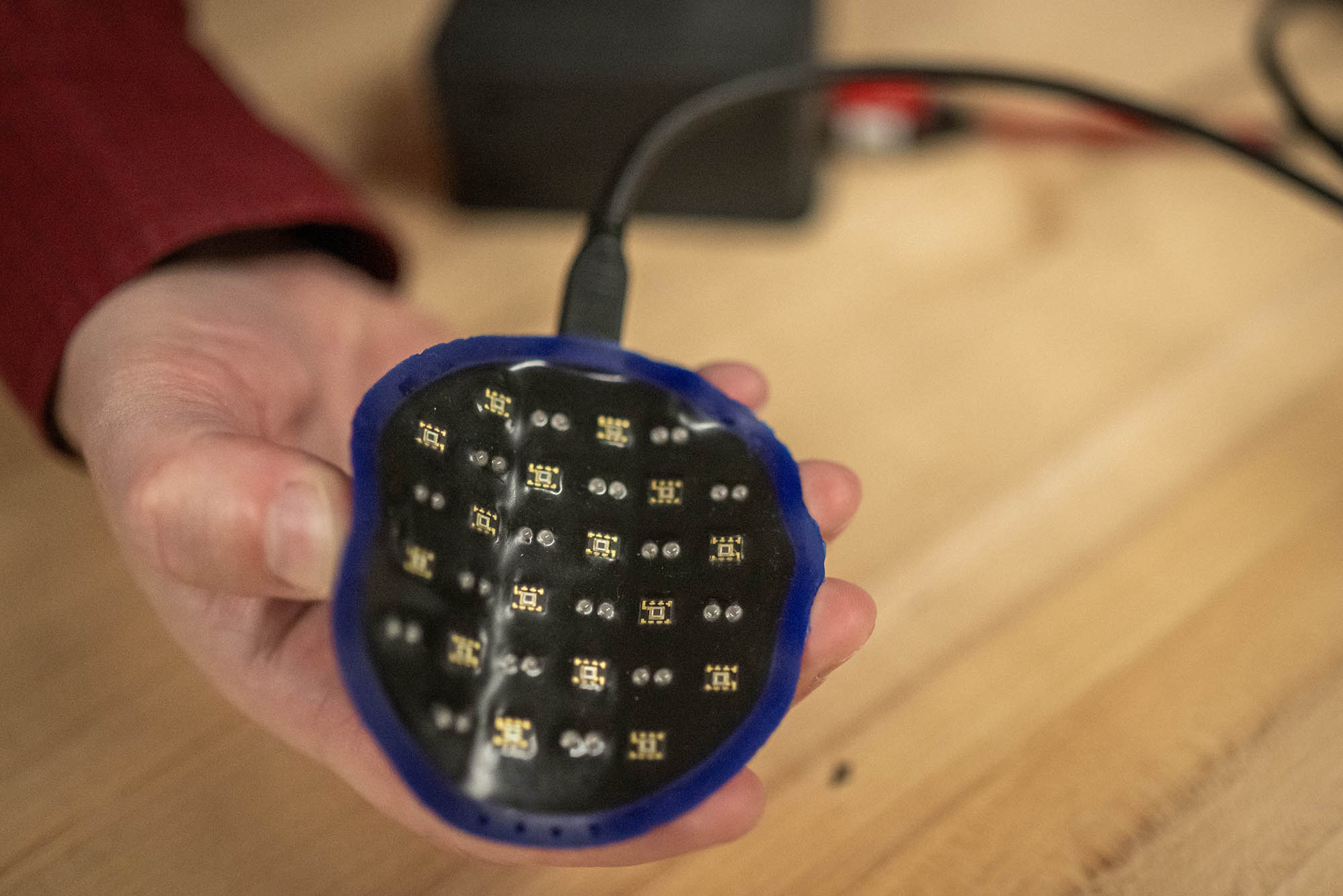
This doesn’t look like a typical blood pressure monitor—but that’s exactly what it is. This device was designed and engineered in Darren Roblyer’s Optical Technologies Lab at BU and uses light to track blood pressure, instead of the standard—and sometimes uncomfortable—cuff.
Using Light to Monitor Blood Pressure and Track Cancer Treatment Progress
Understanding how light interacts with living cells and tissues is the foundation of BU engineer Darren Roblyer’s medical device inventions, which can open up a whole new way of monitoring health
Here’s an experiment: Turn on your phone’s flashlight and place the tip of your finger over the small beam of light. What do you see? Your finger is illuminated, but the light isn’t passing entirely through. You’re looking at what’s called a diffusive glow, which is what happens when all the cells and molecules that make up your finger absorb and scatter the steady beam of light in an instant.
“The light changes direction millions of times so that it turns into a diffuse red glow,” explains Darren Roblyer, a Boston University College of Engineering associate professor of biomedical engineering. Understanding how light interacts with living cells and tissues is the foundation of his work. It might not be as simple as shining a phone flashlight on your finger, but the principles of diffusive glow apply to many of Roblyer’s medical device inventions for tracking health.
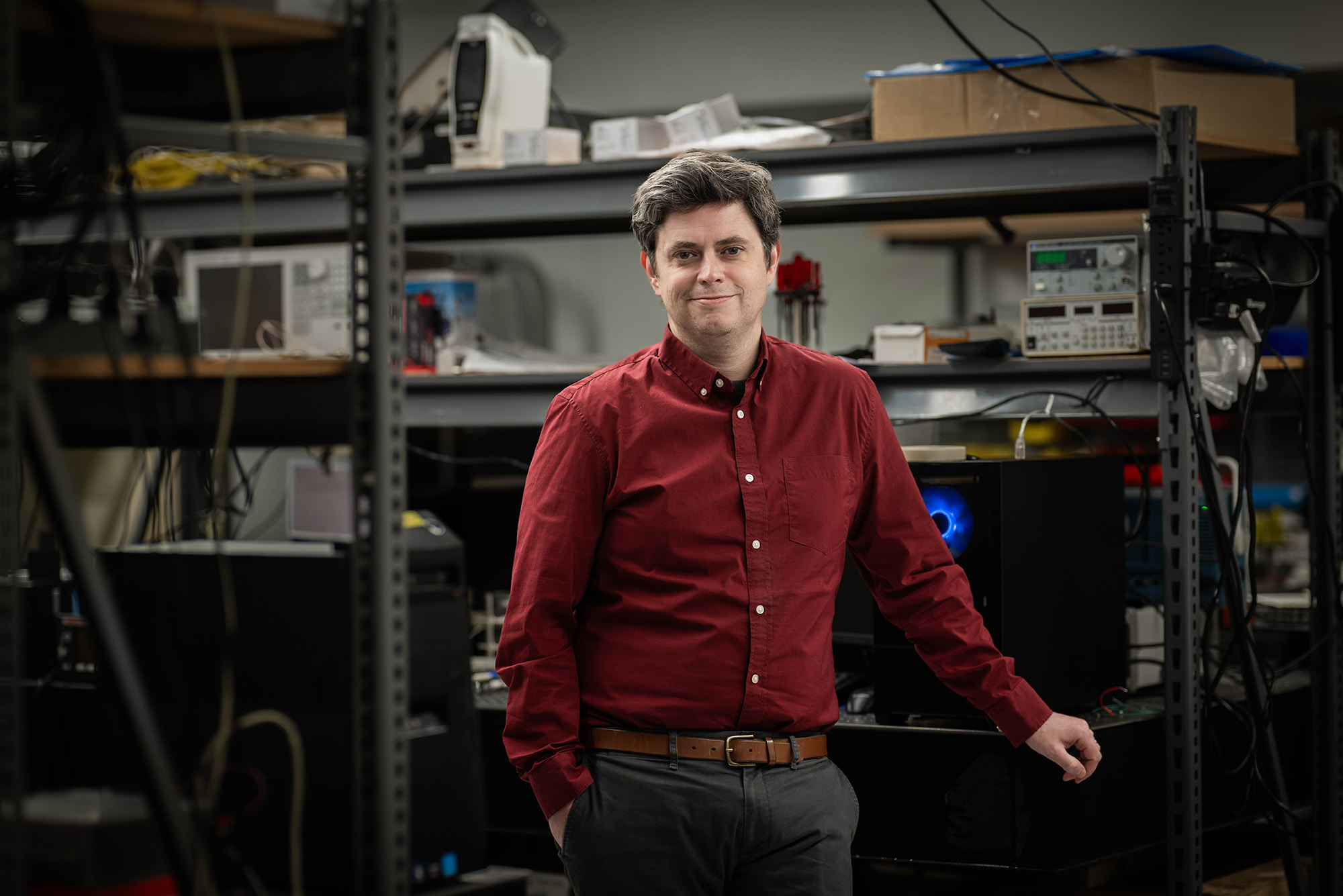
In the Biomedical Optical Technologies Lab, he and his team are testing ways to monitor biological processes—like blood pressure, oxygen levels, and disease progression—with light waves. For example, studying the way different wavelengths of light create patterns when absorbed and scattered can tell Roblyer about the metabolic signals in a person’s blood. Over the past several years, he’s developed a blood pressure monitoring device that does not involve a cuff squeezing your arm, with the aim of getting a more accurate reading than the current, sometimes uncomfortable, options.
“This technology measures the optical effects of what happens when your heart beats,” says Roblyer, who’s also a member of the BU Photonics Center. Each time your heart beats, blood flow speeds up and then slows down, and, at the same time, arteries expand and contract, increasing and decreasing the volume of blood in the arteries. “We’re measuring both of those things, and we are extracting a whole lot of information from those waveforms and then using that to predict blood pressure.”
The device, called speckle contrast optical spectroscopy, uses multiple wavelengths, from visible to near-infrared light (NIR), which is just past what our eyes can see, to monitor blood pressure. The device clips over the finger and straps around the wrist. The team’s latest results, not formally published yet, found that the device took highly accurate, continuous blood pressure measurements on 30 individuals successfully over several weeks.

Current blood pressure devices leave a lot of room for human error, Roblyer says. He points out that taking blood pressure measurements every 15 minutes for 24 hours with his technology, then averaging those results, is much more accurate than a one-time reading in a doctor’s office and better at predicting stroke, heart attack, and cardiovascular disease. It’s common for a physician to prescribe take-home monitors for people who are at risk of hypertension to get readings over the course of 24 hours, “but patients hate it,” Roblyer says.
“The cuff goes off every 15 to 30 minutes, even throughout the night, so it really disrupts sleep,” he says—an issue that gave his team even more incentive to create a cuff-free device.
Tracking Cancer Treatment with Light
Roblyer is also testing a similar type of optical technology—measuring the absorption and scattering of lightwaves—for reading metabolic signals of cancer cells. Specifically, he has been working with Naomi Ko, a BU Chobanian & Avedisian School of Medicine associate professor of medicine and a medical oncologist at Boston Medical Center (BMC), on developing a new tool for monitoring how well breast cancer tumors respond to chemotherapy or radiation treatment. BMC is BU’s primary teaching hospital.
“Despite all the advancements in treatment options for breast cancer, there’s some cases that don’t respond or only partially respond to chemotherapy,” Roblyer says, and current monitoring tools, like mammography, ultrasound, and MRI, “are not particularly good at determining whether a tumor is going to respond.”
The metrics that their device measures—like the concentration and ratio of oxygenated and deoxygenated red blood cells—can be used to predict whether or not a tumor is likely to shrink. More and more, doctors are administering treatments before surgically removing breast cancer tumors, “so monitoring tumor response in real time has great potential benefits,” Ko says. “If we are able to see how much a cancer shrinks in real time, during treatment, it has the potential to help us tailor treatments for patients with breast cancer.”
Ko and Roblyer have been testing the device—which is operated in a similar way to a handheld ultrasound scanner that is moved over the breast tissue—in clinical settings, and plan to continue analyzing its effectiveness over the next year. Eventually, Roblyer wants the device to be smaller and transportable, so that patients can use it at home, and send the readings to their doctors without needing to schedule an appointment.
“This is a technology that is in such early stages, it’s equivalent to where ultrasound was in the 1960s,” Roblyer says. “As knowledge is built, eventually the data will be able to be interpreted and used to make clinical decisions by doctors and nurses.”
There might be a lot more learning, experimenting, and testing to do, but the possibilities are vast. Roblyer’s team is working on a whole suite of other optical technologies, including one to monitor dialysis for kidney disease treatment. They are also in the early stages of creating a device specifically for treating scleroderma—a devastating autoimmune disease that causes inflammation and fibrosis of the skin—that can help doctors determine if drugs are lessening internal fibrosis, since nothing of the sort currently exists.
“One of the most important things I think I do is, as we’re developing these technologies, we’re talking to a lot of physicians, understanding what their unmet needs are, and helping to understand whether our technologies could help,” Roblyer says. “My hope for this work is to make a real impact in the lives of patients.”


Comments & Discussion
Boston University moderates comments to facilitate an informed, substantive, civil conversation. Abusive, profane, self-promotional, misleading, incoherent or off-topic comments will be rejected. Moderators are staffed during regular business hours (EST) and can only accept comments written in English. Statistics or facts must include a citation or a link to the citation.